Table of Contents
Intravenous leiomyomatosis of the uterus: still discovered on anatomopathological examination
Published on: 2nd September, 2022
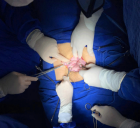
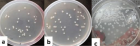
Background: Leiomyomas beyond the uterus are defined by benign smooth muscle cell tumors outside of the uterus. Intravenous leiomyomatosis is a rare type of uterine leiomyoma and is characterized by the formation and growth of benign leiomyoma tissue within the vascular wall. Herein, we present a case of Intravenous leiomyomatosis successfully treated by surgical removal and a review of actual medical recommendations.Case presentation: A 49 - year-old woman, maghrébin, G3 P2, no family history of uterine myomas mentioned, having systemic arterial hypertension, presented to our department with hypogastric pain and abnormal uterine bleeding in the prior five months resulting in anemia which required iron supplementation. On physical examination the vital signs were normal. A palpable mass in the hypogastrium was noted. The rest of the exam was unremarkable. Pelvic ultrasound showed a huge uterus with multiple heterogeneous leiomyomas, including at least one intracavity. Computed tomography scans and magnetic resonance imaging were not done initially due to the unaffordability of the patient. The initial diagnosis was leiomyoma. The decision to perform a total abdominal hysterectomy and bilateral salpingo-oophorectomy was taken. The abdomen was opened by a midline vertical incision. During surgery, multiple subserosal, intramural and submucosal fibroids ranging from 2 cm × 3 cm to 10 cm × 10 cm were seen. On pathological examination, the uterus measured 19 cm in the largest diameter and weighed 1.3 kg. The cut section showed white nodular myometrial masses. Microscopically, intravascular growth of benign smooth muscle cells is found within venous channels lined by endothelium. The diagnosis of Intravenous leiomyomatosis of the uterus without malignant transformation was retained. The patient was monitored for 14 months and subsequent computed tomography did not reveal any evidence of tumor recurrence. The follow-up will be performed annually till the age of menopause.Conclusion: Intravenous leiomyomatosis is a benign, rare and potentially lethal pathology. It especially affects premenopausal women with a history of uterine myoma, whether operated on or not. They require close and prolonged follow-up because of the high risk of recurrence.
Cost-analysis comparison of clinical risk assessment with and without ROMA for the management of women with pelvic masses
Published on: 17th August, 2022
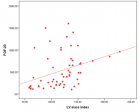
Objective: Pelvic masses can be classified as low risk (likely benign) and high risk (likely malignant) based on an initial clinical risk assessment, which involves a detailed history, physical exam, basic laboratory tests, and imaging. In recent years, the Risk of Ovarian Malignancy Algorithm (ROMA), which combines CA125, HE4 and menopausal status, has emerged as a powerful tool in the classification of pelvic masses and triage of patients to either a generalist gynecologist or a gynecologic oncologist for management. The objective of this study was to evaluate whether the use of ROMA, alone or in combination with Initial Clinical Risk Assessment (ICRA), provides cost savings compared to triage based on ICRA alone.Methods: A health-economic decision model was developed to assess clinical and cost differences associated with three different clinical pathways of risk assessment for a pelvic mass: ICRA alone, ROMA alone, or ICRA + ROMA in combination. Using previously reported accuracy rates and patient characteristics from a prospective, multicenter, blinded clinical trial, total healthcare costs were modeled for each clinical pathway using the Medicare 2020 reimbursement rates.Results: A total of 461 patients with pelvic masses were included with 10.4% ultimately diagnosed with epithelial ovarian cancer. Total healthcare costs for patients with benign disease, EOC, or low malignant potential tumors (LMP) (n = 441) triaged using ROMA alone were 3.3% lower than when triaged using ICRA alone. While lab costs increased 55% using ROMA, the use of ROMA alone resulted in a 4% decrease in laparoscopy costs and a 3.1% decrease in laparotomy costs compared with ICRA alone. Similarly, total costs associated with a combination of ICRA + ROMA were 3.9% lower than total costs associated with ICRA alone. The model also predicted a 63% reduction in repeat surgeries resulting from false negative ICRA when using ROMA to triage patients.Conclusion: Triage of women with pelvic masses using the more sensitive ROMA score lowers overall healthcare costs compared to ICRA alone. With fewer false negative results than ICRA alone, the ROMA score improves initial detection of malignancy and reduces second surgical treatments in women with pelvic masses.
Patient, disease and surgeon predictors of successful bilateral sentinel lymph node mapping for endometrial cancer: A retrospective, multicenter analysis
Published on: 14th July, 2022
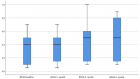
Objective: Sentinel lymph node mapping is an acceptable standard for lymph node evaluation in patients with endometrial cancer. The purpose of this study was to evaluate the adoption of this technique at two academic institutions, including which patient and disease features are associated with rates of successfully identifying sentinel lymph nodes with fluorescent mapping. In addition, we sought to characterize if and how surgeons experience the technique related to successful bilateral sentinel lymph node mapping. Methods: A retrospective chart review was performed of patients at two academic institutions who underwent sentinel lymph node mapping prior to a minimally invasive hysterectomy for endometrial cancer over the first 30 months during which the technique was adopted at each institution. A modified Poisson regression model was used to determine the relationships between patient, disease, and surgeon factors on outcomes of sentinel lymph node mapping. Results: A total of 460 charts were reviewed. The mean age was 64 and the median body mass index was 34.2. The most disease was stage I (83%), endometrioid (89%), and Grade I (64%). The bilateral sentinel lymph node mapping success rate was 65%, while unilateral or bilateral success occurred in 91% of cases. Sentinel lymph node mapping was significantly more likely to be successful in premenopausal women (RR 1.25; 95% CI 1.07 - 1.46; p = 0.005) and Asian women (RR 1.48; 95% CI 1.3-1.68; p < 0.001). BMI was not significantly predictive of mapping success (RR 1.03; 95% CI 1.00 - 1.07; p = 0.05). Increasing surgeon experience with the technique did predict successful bilateral sentinel lymph node mapping (RR 1.02; 95% CI 1.00 - 1.03; p = 0.02).Conclusion: Premenopausal status and surgeon experience with the technique increases the likelihood of bilateral sentinel lymph node detection for endometrial cancer.

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."