More Information
Submitted: March 31, 2025 | Approved: April 10, 2025 | Published: April 11, 2025
How to cite this article: Soukaina M, Oumaima M, Amina E, Najia Z, Aziz S, Aziz B. Validation of Prognostic Scores for Attempted Vaginal Delivery in Scar Uterus. Clin J Obstet Gynecol. 2025; 8(2): 023-029. Available from:
https://dx.doi.org/10.29328/journal.cjog.1001185
DOI: 10.29328/journal.cjog.1001185
Copyright license: © 2025 Soukaina M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Obstetrics; Cesarean section; Public health
Validation of Prognostic Scores for Attempted Vaginal Delivery in Scar Uterus
Mouiman Soukaina*, Mourran Oumaima, Etber Amina, Zeraidi Najia, Slaoui Aziz and Baydada Aziz
Gynaecology-Obstetrics and Endoscopy Department, Maternity Souissi, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco
*Address for Correspondence: Mouiman Soukaina, Gynaecology-Obstetrics and Endoscopy Department, Maternity Souissi, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco, Email: [email protected]
Introduction: The rise in cesarean section rates globally has led to a growing population of women with uterine scars, necessitating more targeted obstetric care in subsequent pregnancies. These women are faced with the decision of attempting vaginal delivery after cesarean section (VBAC) or opting for an elective repeat cesarean section. The likelihood of a VBAC depends on various factors both maternal and fetal, gathered in two known scores Grobman and Zhang, utilizing them could make VBAC successful and more widely attempted. This study aims to validate the prognostic of these scores in a Moroccan population.
Objectives:
- Validate the international predictive scores (Grobman and Zhang) for the probability of a successful VBAC in the Moroccan population.
- Explore additional criteria specific to the Moroccan population and develop a simplified VBAC score.
Results:
- Out of 2,973 women with a cesarean history, 313 attempted TOLAC, 79% of these attempts were successful VBAC.
- The characteristics of successful VBAC included lower BMI, previous vaginal birth, lower estimated fetal weight, younger maternal age, and more favorable cervical conditions at admission.
- The Grobman and Zhang scores showed good predictive accuracy, with both models achieving 82.2% accuracy.
- When dividing women into groups based on predicted success (using both Grobman and Zhang scores), significant differences were found in success rates across different probability categories.
Conclusion: Both Grobman and Zhang’s models were effective in predicting VBAC success in the Moroccan population, with a slight preference for the Zhang model. However, further research is needed to validate these models in clinical practice. It could involve developing a more population-specific model.
Constant developments in the field of obstetrics have led to a steady increase in the cesarean section rate, both in Morocco and the rest of the world [1-3]. This change in practice has led to the emergence of a large population of women with uterine scars, requiring more targeted obstetric care during their subsequent pregnancies. These women must choose between two delivery options: attempted vaginal delivery after caesarean section (VBAC) or elective repeat cesarean section. The likelihood of a successful VBAC depends on many factors and varies according to the individual characteristics of each woman. Researchers have confirmed that VBAC could be more widely attempted if its success could be predicted [4].
Obstetricians used a variety of methods to counsel women about their likelihood of having a VBAC [5]. The most naïve strategy (simple but not allowing for individualized prediction) has been to inform women of the reported success rate in the general population of women who have undergone VBAC as a whole. The other, more individualized approach is for an obstetrician to assess the extent to which a given woman's probability differs from that of the general population, using the various factors associated with successful VBAC. But this approach is essentially qualitative and does not allow a probability of success to be calculated [6].
Predictive models have been proposed to reproduce a quantitative value of the probability of successful VBAC while considering the individual demographic characteristics of women [7]. Among the various models available for this purpose, the most widely used and accepted is the one proposed in 2007 by Grobman, et al. [8], based on an American cohort of 11,000 women who had undergone VBAC, and updated in 2022 [7]. The nomogram considers maternal parameters such as age, maternal BMI, history of vaginal birth or VBAC, and indication for previous caesarean section. The predictive accuracy of the nomogram has been studied and established in American [9], Japanese [10], European [11], French [12] and very recently Indian [13] cohorts; however, ambiguity reigns as to its generalizability in populations with different demographic profiles. Several other scores have subsequently been developed. The most recent, which its authors consider superior to Grobman's score, is the one created by Zhang, et al. [3] in 2020.
In this retrospective study, the predictive scores of Grobman and Zhang were applied to a Moroccan population cohort, and the estimated probability of success of VBAC was compared with the actual success rate obtained in the population.
Objectives
The main objective of our study was to validate the international predictive scores of Grobman, et al. [7] and Zhang, et al. [3] on the probability of successful vaginal delivery after caesarean section in our Moroccan population.
The secondary objectives of our study were to:
- Look for other criteria specific to our Moroccan population.
- Create our simplified score on the probability of successful vaginal delivery after cesarean section.
Our assumptions were as follows:
- The predictive scores are applicable to the Moroccan population.
- The Chinese score is more precise than the American one, as it considers not only the patient's BMI but also the estimated fetal weight.
Type of study
Our study is part of a retrospective study, within the Souissi Maternity Hospital of the Ibn Sina University Hospital in Rabat, spread over a 24-month period (from January 1st, 2022 to December 31st 2023).
Three tasks were carried out:
- Data collection: All records of patients admitted to the Souissi Maternity Hospital for delivery with a previous c section during the study period were analyzed and recorded in the form of a Google Form questionnaire and an Excel table.
- Application of predictive scores: We then applied Grobman's and Zhang's predictive scores to each file, which we added to their Google form and Excel table.
- Statistical data analysis: Based on the data collected, a database was created using Excel 2022 software.
The comparative descriptive analysis was represented using numbers and percentages, and we performed the statistical analysis using the online software biostaTGV: https://marne.u707.jussieu.fr/biostatgv/.
Categorical variables were compared using Chi-2 and Fisher's exact tests. A 95% confidence interval was used. Tests were considered significant for a "p - value" less than or equal to 0.05.
The data thus collected were analyzed to establish the correlation between the predictive score and:
Delivery route The use of certain new factors.Study population
We included all deliveries on scar uterus occurring between January 1, 2022, and December 31, 2023, at the Maternity Souissi of the CHU Ibn Sina in Rabat, meeting the following criteria:
- Delivery after 37 weeks gestation
- Single live fetus
- Attempted spontaneous vaginal delivery
- Single lower uterine segment cesarean section (LOCUS)
- Absence of recurrence of indications for previous cesarean section in this pregnancy before labor: abnormal fetal position, placenta previa, Oligohydramnios, severe PE, placental abruption and twin pregnancy.
- EFW < 4000g
- Ultrasound analysis of the caesarean scar
Patients with the following criteria were excluded
- Obstetrical history: twice scared uterus, uterine rupture, corporal scarring
- Absolute CI for vaginal delivery
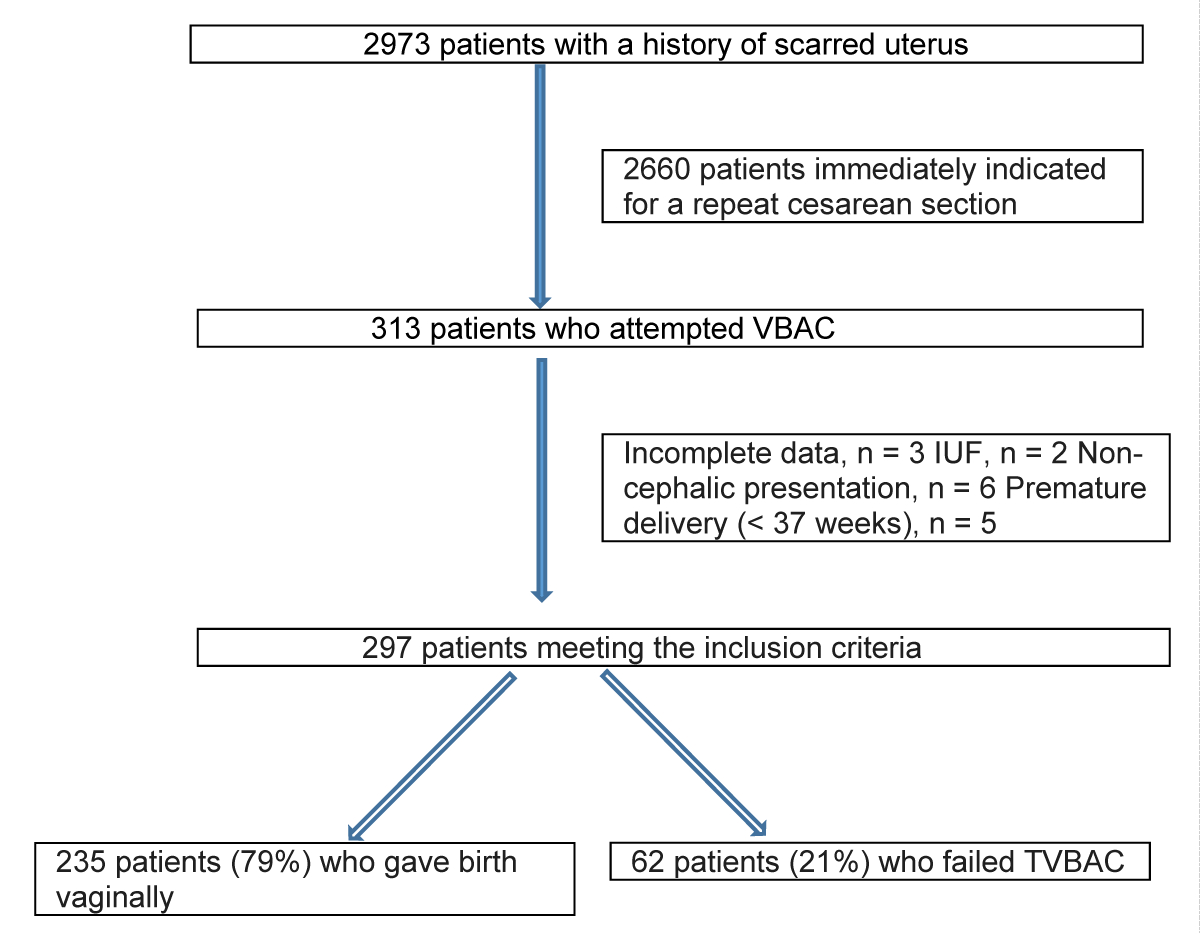
During the study period, 2,973 women had a history of a caesarean section, and only 313 women had a trial of labor after c section (TOLAC); the rate of VBAC was 10.5%. 292 women (94.9%) met the inclusion criteria, and complete data were available for these women. The characteristics of these women are presented in Table 1. A total of 235 women underwent TOLAC and 61 women failed at it, with a success rate of 79% (Figure 1).
| Table 1: Characteristics of patients attempting vaginal delivery. Data are expressed as mean ± standard deviation, median (IQR) or n (%). | ||||
| Variable | Total (n = 297) | Success (n = 235) | Failure (n = 62) | p - value |
| Maternal age (years) | 26 ± 4.00 | 25.8 ± 4.10 | 26.2 ± 3.47 | 0.553 |
| Maternity residence | 0.834 | |||
| Rabat | 120 | 103 | 23 | |
| Other towns in the RSK province | 46 | 21 | 7 | |
| Rural environment | 131 | 111 | 32 | |
| Gravidity | 3 (2, 4) | 3 (2, 4) | 3 (2, 4) | 0.585 |
| Parity | 1 (1, 1) | 1 (1, 1) | 1 (1, 1) | 0.963 |
| Recurrent indication for caesarean section | 13 (4.4) | 9 (3.8) | 3 (4.8) | 0.092 |
| Any previous vaginal birth | 38 (12.7) | 33 (14.0) | 5 (8.1) | < 0.001 |
| Vaginal birth after previous caesarean section | 19 (6.4) | 18 (7.7) | 1 (1.6) | < 0.001 |
| BMI at last prenatal visit (kg/m2) | 27.78 ± 2.53 | 26.07 ± 1.97 | 29 ± 2.78 | < 0.001 |
| Gestational age at delivery (weeks) | 38.93 ± 1.17 | 38.91 ± 1.20 | 39.03 ± 1.11 | 0.047 |
| Preeclampsia | 11 (3.7) | 8 (3.4) | 3 (4.8) | 0.008 |
| Cervical effacement on admission (10%) | 8.73 ± 1.56 | 9.5 ± 1.06 | 7.68 ± 2.46 | < 0.001 |
| Cervical dilatation on admission (cm) | 1.87 ± 1.61 | 1.97 ± 1.47 | 0.78 ± 1.27 | < 0.001 |
| Admission presentation level | 3 (3, 3) | 3 (3, 3) | 3 (2, 3) | < 0.001 |
| Work induction | 9 (3.0) | 4 (1.7) | 5 (8.1) | 0.002 |
| Maternal size | 161.87 ± 4.52 | 162.17 ± 4.29 | 159.73 ± 4.23 | 0.006 |
| Estimation of fetal weight | 3312 ± 363.76 | 3283 ± 374.75 | 3437 ± 271.13 | 0.002 |
| Time interval since previous caesarean section (months) | 63.05 ± 38.58 | 64.52 ± 37.46 | 61.68 ± 39.58 | 0.547 |
| Perinatal care registration | 183 (61.6) | 147 (62.5) | 37 (59.7) | 0.120 |
| Labor analgesia | 62 (20.9) | 50 (21.2) | 12 (19.4) | 0.192 |
| Indications for previous caesarean section | 0.013 | |||
| Social factors | 27 (9.0) | 21 | 6 (9.6) | |
| Fetal malposition | 34 (11.4) | 25 | 9 (14.5) | |
| Macrosomia | 39 (13.1) | 29 | 10 (16.1) | |
| Anomalies in the work stages | 56 (18.9) | 41 | 15 (24.2) | |
| Fetal suffering | 52 (27.6) | 41 (17.4) | 11 (17.7) | |
| Abnormal amniotic fluid volume | 23 (17.5) | 17 (7.2) | 6 (9.6) | |
| Prolonged pregnancy, ≥42 weeks | 7 (2.4) | 3 | 4 (6.4) | |
| Serious complications of pregnancy or maternal illness | 48 (16.12) | 37 (15.7) | 11 (17.7) | |
| Circular cord, ≥3 cycles | 11 (3.7) | 7 (3.0) | 4 (6.4) | |
Figure 1: Diagram showing the selection of the target population.
Compared with the group that failed TOLAC, parturients in the successful group were less likely to have recurrent indications for caesarean section; in addition, these women were more likely to have had a previous vaginal birth, a previous vaginal birth after caesarean section, to be taller, to have a lower BMI at the last prenatal visit, a lower estimated fetal weight, a younger estimated gestational age at delivery, lower rates of preeclampsia and induction of labor, as well as higher cervical effacement and cervical dilation at admission, and to have a lower level of presentation at admission but also a birth (all p - value < 0,05). The difference in the distribution of indications for previous caesarean section between the two groups was also significant (p - value < 0.05). However, there were no significant differences in the distribution of maternal age, maternal residence, time interval since previous cesarean section, perinatal care registration or labor analgesia rate between the TOLAC pass and fail groups (all p - value > 0.05).
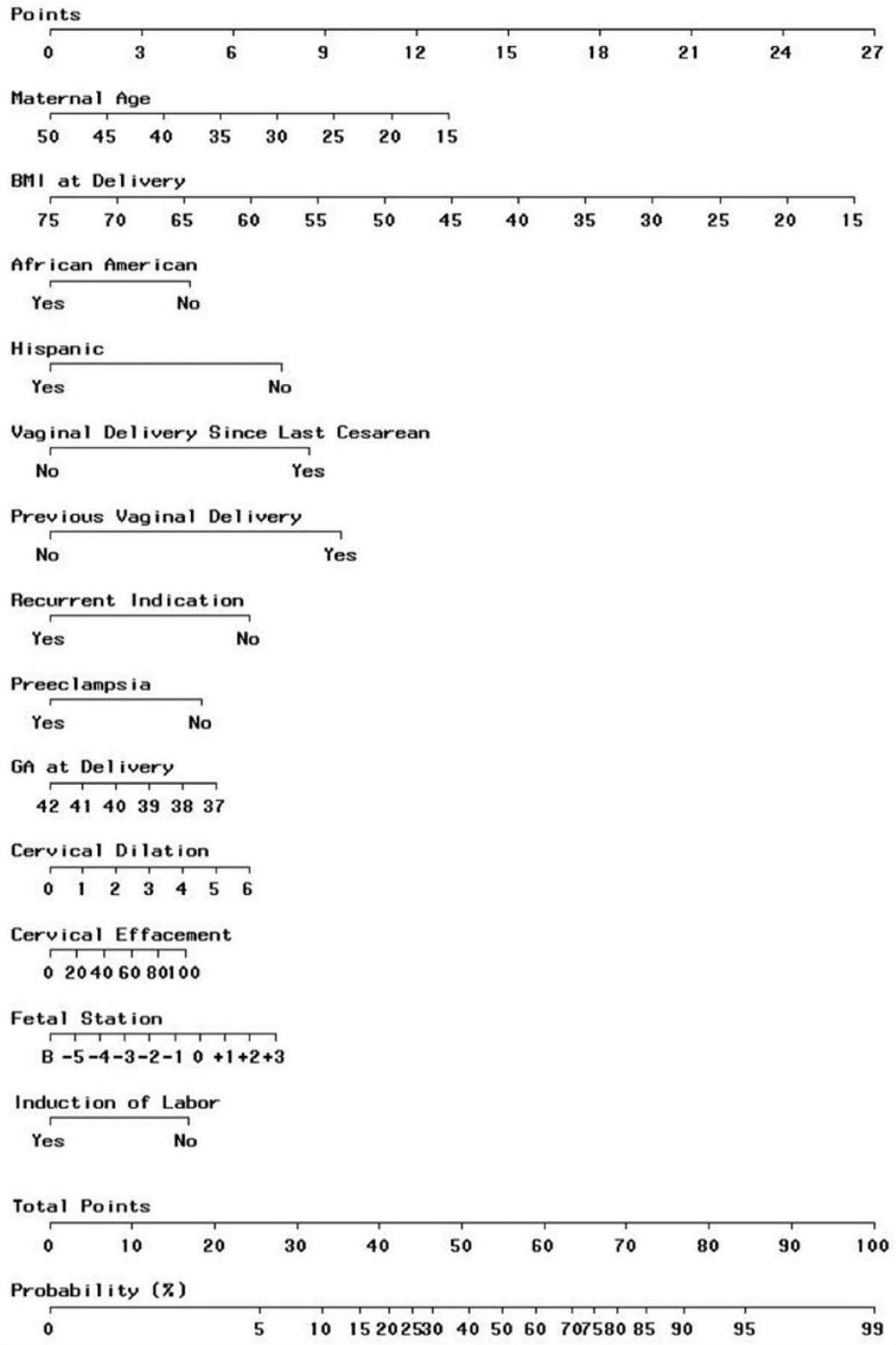
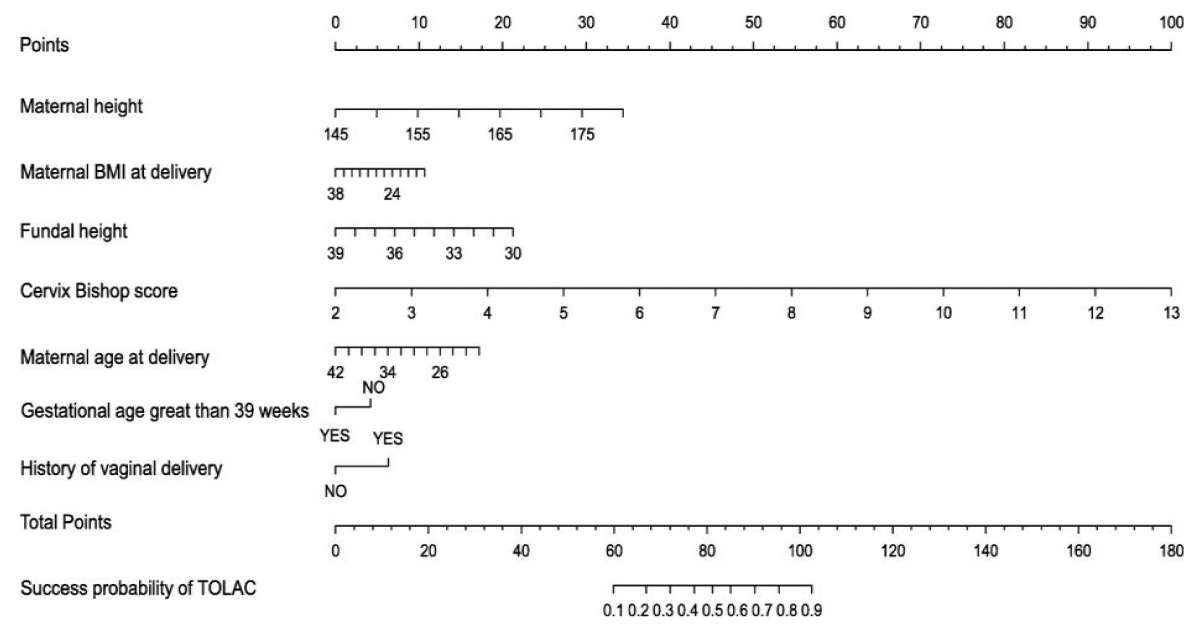
Any previous “vaginal birth” and "cervical effacement on admission" were both positively associated with VBAC (all p < 0.05). “Recurrent cesarean indications", "BMI at last prenatal visit", "preeclampsia" and "induction of labor" were all negatively associated with VBAC (all p < 0.05). In addition, "vaginal birth after previous caesarean section" was positively associated with VBAC with marginal significance (p = 0.059). We added five new background variables used in the Zhang, et al. score [3] (maternal height, estimated fetal weight, time interval since previous caesarean section, perinatal care registration and labor analgesia) to the model. After stepwise regression analysis, "recurrent cesarean indications", "any previous vaginal birth", "vaginal birth after previous cesarean", "BMI at last prenatal visit", "preeclampsia", "cervical effacement on admission", "induction of labor", "maternal size" and "estimated fetal weight" were included in the VBAC prediction model. Both "maternal size" and "estimated fetal weight" were considered as two additional predictors for VBAC (Figures 2,3).
Figure 2: Modified score from Grobman, et al. [3].
Figure 3: Zhang, et al. score [9].
The probability of successful VBAC predicted by the Grobman, et al. score [7] ranged from 23% to 98% for the women in the study population. The mean probability of success calculated for the entire population was 78.3%, whereas the actual VBAC rate observed in the present study was 79.1%.
Women were divided into 3 groups according to Grobman probability: < 50% probability (7.7%), 50% - 75% probability group (37%) and > 75% probability group (55.2%). Significant differences in VBAC and cesarean section rates were observed at different predicted probabilities (p = 0.003). For women in the probability > 75% group, the mean predicted Grobman probability was 91.5%, while the actual observed VBAC success was 93.3% (p = 0.003). For women in the 50% - 75% probability group, the mean predicted probability was 66.9%, and the observed VBAC success was 68.2% (p = 0.008), compared with women in the 50% probability group who had a mean predicted probability of 38.8% but ended up with a lower observed VBA success rate of 30.4% (p = 0.018).
The probability of successful VBAC predicted by the Zhang, et al. score (3) ranged from 13% to 99% for the women in the study population. The mean probability of success calculated for the entire population was 78.1%, whereas the actual VBAC rate observed in the present study was 79.1%.
Women were divided into 3 groups according to Zhang probability: < 50% probability (9.1%), 50% - 75% probability group (34%) and > 75% probability group (56.9%). Significant differences in VBAC and cesarean section rates were observed at different predicted probabilities (p = 0.002). For women in the > 75% probability group, the mean predicted Zhang probability was 91.6%, while the actual observed VBAC success was 94.1% (p = 0.003). For women in the 50% - 75% probability group, the mean predicted probability was 66.9%, and the observed VBAC success was 66.3% (p = 0.002), compared with women in the 50% probability group who had a mean predicted probability of 35.5% but ended up with a lower observed VBAC success rate of 33.3% (p = 0.004).
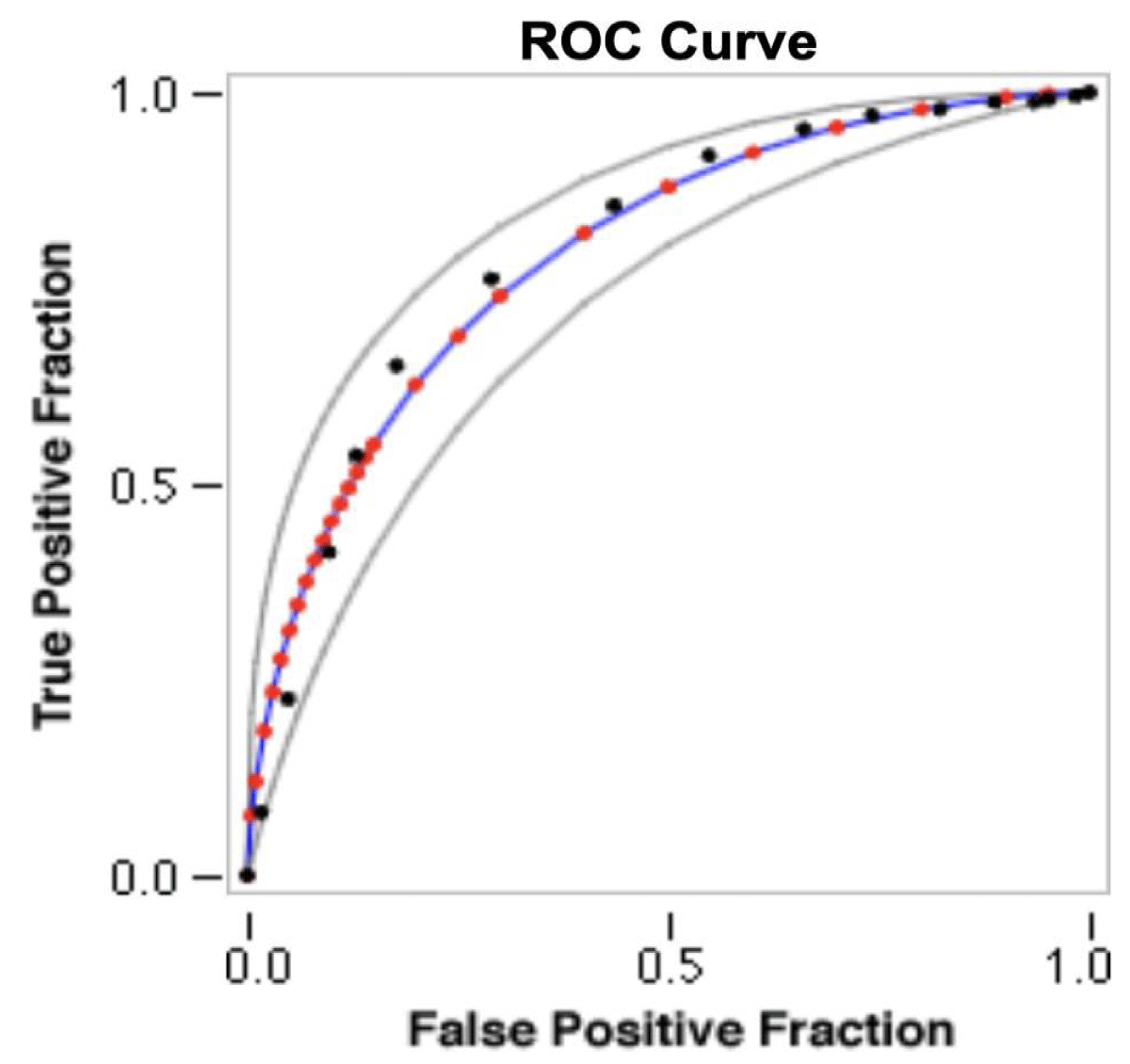
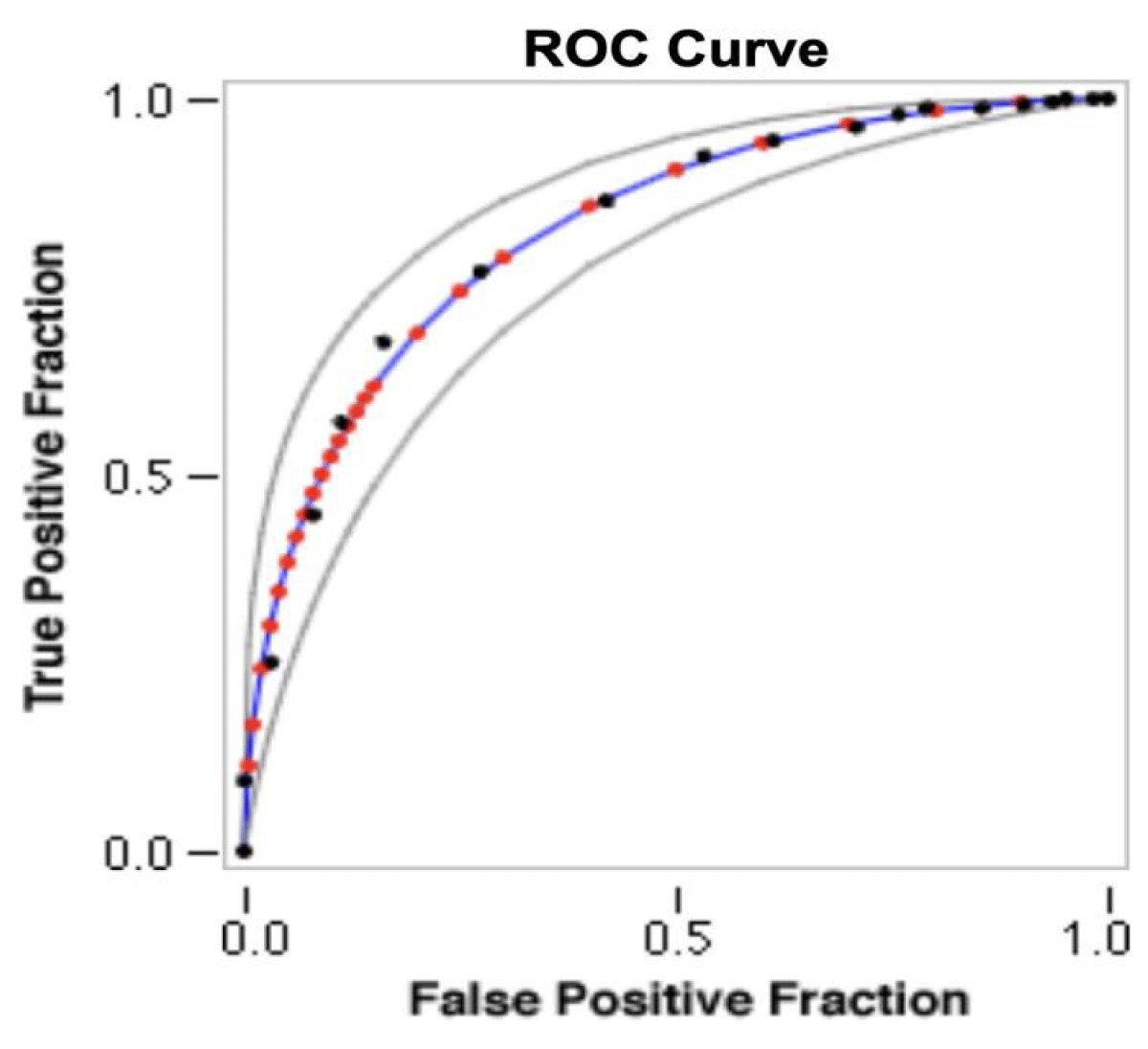
ROC curves (Figure 4 and 5) were obtained via the John Hopkins Medicine online ROC curve calculator [14]. Grobman's predicted TOLAC success probabilities were calculated with an accuracy of 82.2% (adjusted AUC 0.795 and empirical AUC 0.799, 95% CI). TOLAC success probabilities predicted by Zhang were calculated with an equal accuracy rate of 82.2% but with a larger area under the ROC curve (adjusted AUC 0.826 and empirical AUC 0.825, 95% CI .
Figure 4: Receiver-operator curve for prediction of vaginal delivery after caesarean section using the Grobman model. Legend for the ROC graph: - RED symbols and BLUE line: ROC curve adjusted. - GREY lines: 95% confidence interval of the fitted ROC curve. - BLACK symbols: Points making up the empirical ROC curve.
Figure 5: Receiver-operator curve for prediction of vaginal delivery after caesarean section with Zhang model. Legend for the ROC graph: - RED symbols and BLUE line: ROC curve adjusted. - GREY lines: 95% confidence interval of the fitted ROC curve. - BLACK symbols: Points making up the empirical ROC curve.
In our comparative analysis with data from the literature, we found a success rate for vaginal deliveries or attempted labor after cesarean section (VB/TOLAC) of 79% in our study. In an earlier study in China, a slightly higher success rate was reported, reaching 85.2% [15], while a study in India reported a slightly lower rate of 54.8% [13]. These results suggest a general consistency in VB/TOLAC success rates between different populations, while indicating potential variations that could be attributed to factors such as clinical protocols, patient demographics or region-specific obstetric practices.
In our study, a univariate analysis was carried out to examine factors associated with the success rate of VBAC/TOLAC. The results showed similarities with observations in the existing literature. Indeed, a history of VB, lower body mass index (BMI), lower fetal weight, more advanced effacement and dilation on admission, and absence of preeclampsia (PE) were associated with a higher success rate, which is consistent with previous data [13,15].
However, some factors showed different associations compared with the literature. For example, maternal age and the time interval between the last cesarean section and the administration of analgesia for labor were significantly different [16]. These variations could reflect differences in the composition of the study sample, local clinical practices or other contextual factors specific to our study population. Multivariate analysis could be undertaken to further elucidate these relationships and their impact on obstetric outcomes.
We evaluated both Zhang and Grobman [2,3] models on our sample population. The results showed that both models were effective, with ROC curves indicating high sensitivity and specificity. These performances are consistent with previous studies carried out in China and India [13,15]. Our study also revealed that the Zhang model showed a slight improvement over the Grobman model. This improvement is attributable to the Zhang model's use of additional factors not considered by the Grobman model, leading to greater accuracy in predictions.
Our study has several strengths. Firstly, the research design effectively avoids observational bias. Secondly, patient information was comprehensive and robust, including clinical history, patient demographics and early factors, enabling the association of several factors to be investigated. Thirdly, this was a retrospective study conducted in a single center in a homogeneous population.
Our study has several limitations that should be considered.
First, although we included a substantial sample size over a two-year period, this duration may still be insufficient to fully capture the variability and complexity of the phenomenon under investigation.
Second, the monocentric design—conducted in a single hospital in Morocco—limits the generalizability of our findings. The demographic and clinical characteristics of our study population may not reflect the diversity observed across other regions of the country. A multicenter approach involving hospitals from various cities would allow for a more representative assessment of the Moroccan population and enhance the external validity of the results.
Third, the use of international predictive scores (Grobman and Zhang) in a local context may be problematic, as these models were originally developed in different populations and healthcare systems. Although our findings indicate acceptable predictive accuracy, these scores may not fully account for population-specific factors relevant to Moroccan women. As a result, we propose the development of a tailored predictive model based on a prospective, multicenter study. Such a model would be better suited to the local context and could potentially improve the accuracy and clinical utility of VBAC prediction in Moroccan obstetric care.
The use of scores is crucial for informed decision-making on mode of delivery, improving the quality of care, and systematically assessing the potential risks associated with each mode of delivery, which is essential for ensuring the safety and well-being of mother and child.
The Zhang and Grobman models have demonstrated their effectiveness in our population, with a slight preference for the Zhang model in terms of performance. However, a future large-scale prospective study is needed to validate these prediction models in a clinical setting.
Interest of the study
Predictive scores for the probability of vaginal delivery, such as those developed by Grobman or Zhang, are valuable tools in obstetric practice for several reasons:
- Informed decision-making: These scores provide healthcare professionals with quantitative estimates of the likelihood of a successful vaginal delivery. This information enables them to advise pregnant women more effectively on their birthing options, including the potential risks and benefits associated with attempting a vaginal delivery after a caesarean section versus an iterative caesarean section.
- Individualized care: By considering various maternal and fetal factors, predictive scores help to tailor care plans to each patient's specific circumstances. This individualized approach improves the accuracy of clinical decision-making, leading to better outcomes and increased patient satisfaction.
- Risk assessment: Predictive scores are also linked to the likelihood of maternal-fetal morbidity. This information guides resource allocation and facilitates early intervention for patients who may require additional support during labor or delivery.
- Quality improvement: Healthcare professionals can use these scores to monitor and evaluate the effectiveness of obstetric interventions and protocols over time. By tracking results against predicted probabilities, institutions can identify areas for improvement and implement targeted strategies to optimize care delivery.
Overall, predictive scores for the likelihood of vaginal delivery play a crucial role in improving patient-centered care, promoting shared decision-making and improving clinical outcomes in obstetrics.
Predictive scores for the probability of vaginal delivery, such as those developed by Grobman or Zhang, offer a solid basis for informed decision-making in obstetrics. By providing quantitative estimates of the potential success of vaginal delivery, these tools enable healthcare professionals to advise pregnant women on their birthing options, thus promoting an individualized approach and management tailored to each patient. In addition, these scores enable a precise assessment of maternal and fetal risks, facilitating the allocation of resources and the identification of areas for improvement to optimize care delivery and improve the quality of clinical outcomes in obstetrics
Consent: The consent of the patients was obtained to carry out this studyEthical approval: This study is exempt from ethical approval from our institute
Patients and public involvement: This study did not involve direct patient participation. Data was collected retrospectively from patient records, ensuring patient privacy while allowing for a comprehensive analysis of factors influencing the success of normal delivery after a prior Cesarean section. This approach allowed us to efficiently evaluate existing prediction models using real-world clinical data.
- Angolile CM, Max BL, Mushemba J, Mashauri HL. Global increased cesarean section rates and public health implications: A call to action. Health Sci Rep. 2023;6(5):e1274. Available from: https://doi.org/10.1002/hsr2.1274
- Grobman WA, Lai Y, Landon MB, Spong CY, Leveno KJ, Rouse DJ, et al. Development of a Nomogram for Prediction of Vaginal Birth After Cesarean Delivery. Obstet Gynecol [Internet]. 2007;109(4). Available from: https://journals.lww.com/greenjournal/fulltext/2007/04000/development_of_a_nomogram_for_prediction_of.5.aspx
- Zhang HL, Zheng LH, Cheng LC, Liu ZD, Yu L, Han Q, et al. Prediction of vaginal birth after cesarean delivery in Southeast China: a retrospective cohort study. BMC Pregnancy Childbirth. 2020;20(1):538. Available from: https://doi.org/10.1186/s12884-020-03233-y
- Cunningham FG, Bangdiwala SI, Brown SS, Dean TM, Frederiksen M, Rowland Hogue CJ, et al. NIH consensus development conference draft statement on vaginal birth after cesarean: new insights. NIH Consens State Sci Statements. 2010;27(3):1-42. Available from: https://pubmed.ncbi.nlm.nih.gov/20228855/
- Chaillet N, Bujold E, Dubé E, Grobman WA. Validation of a Prediction Model for Vaginal Birth After Caesarean. J Obstet Gynaecol Can. 2013;35(2):119-24. Available from: https://doi.org/10.1016/s1701-2163(15)31015-x
- Habak PJ, Khaparde G, Vadakekut ES. Vaginal Birth After Cesarean Delivery. [Updated 2025 Feb 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507844/
- Grobman WA, Sandoval G, Rice MM, Bailit JL, Chauhan SP, Costantine MM, et al. Prediction of vaginal birth after cesarean delivery in term gestations: a calculator without race and ethnicity. Am J Obstet Gynecol. 2021;225(6):664.e1-664.e7. Available from: https://doi.org/10.1016/j.ajog.2021.05.021
- Grobman WA. Rates and prediction of successful vaginal birth after cesarean. Semin Perinatol. 2010;34(4):244-8. Available from: https://doi.org/10.1053/j.semperi.2010.03.003
- Costantine MM, Fox K, Byers BD, Mateus J, Ghulmiyyah LM, Blackwell S, et al. Validation of the prediction model for success of vaginal birth after cesarean delivery. Obstet Gynecol. 2009;114(5):1029‑33. Available from: https://doi.org/10.1097/aog.0b013e3181bb0dde
- Yokoi A, Ishikawa K, Miyazaki K, Yoshida K, Furuhashi M, Tamakoshi K. Validation of the prediction model for success of vaginal birth after cesarean delivery in Japanese women. Int J Med Sci. 2012;9(6):488‑91. Available from: https://doi.org/10.7150/ijms.4682
- Schoorel ENC, Melman S, van Kuijk SMJ, Grobman WA, Kwee A, Mol BWJ, et al. Predicting successful intended vaginal delivery after previous caesarean section: external validation of two predictive models in a Dutch nationwide registration-based cohort with a high intended vaginal delivery rate. BJOG. 2014 Jun;121(7):840‑7; discussion 847. Available from: https://doi.org/10.1111/1471-0528.12605
- Haumonte JB, Raylet M, Christophe M, Mauviel F, Bertrand A, Desbriere R, et al. French validation and adaptation of the Grobman nomogram for prediction of vaginal birth after cesarean delivery. J Gynecol Obstet Hum Reprod. 2018;47(3):127‑31. Available from: https://doi.org/10.1016/j.jogoh.2017.12.002
- Bhardwaj M, Gainder S, Chopra S, Bagga R, Saini SS. Validation of Grobman’s graphical nomogram for prediction of vaginal delivery in Indian women with previous caesarean section. Eur J Obstet Gynecol Reprod Biol X. 2023;18:100188. Available from: https://doi.org/10.1016/j.eurox.2023.100188
- Eng J. ROC analysis: web-based calculator for ROC curves. Baltimore: Johns Hopkins University. Available from: http://www.jrocfit.org. Disponible sur: http://www.rad.jhmi.edu/jeng/javarad/roc/JROCFITi.html
- Xu P, Feng Y, Shen H, Luo J, Tao Y. Verification a model of predicting vaginal birth after cesarean delivery in Chinese pregnant women. Medicine (Baltimore) [Internet]. 2019;98(52). Available from: https://journals.lww.com/md-journal/fulltext/2019/12270/verification_a_model_of_predicting_vaginal_birth.16.aspx
- Zewdu D, Tantu T, Degemu F, Abdlwehab M. Association between the stage of labour during caesarean delivery with adverse maternal and neonatal outcomes among referred mothers to tertiary centres in resource-limited settings. BMJ Open. 2023 Nov 1;13(11):e077265. Available from: https://doi.org/10.1136/bmjopen-2023-077265