More Information
Submitted: March 26, 2025 | Approved: April 07, 2025 | Published: April 08, 2025
How to cite this article: Elimam AMA, Babbiker IM, Farah RME, Abbas AS, Sayed OMA. Huge Mucinous Cyst Adenoma, Case Report Series. Clin J Obstet Gynecol. 2025; 8(2): 019-022. Available from:
https://dx.doi.org/10.29328/journal.cjog.1001184
DOI: 10.29328/journal.cjog.1001184
Copyright license: © 2025 Elimam AMA, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Ovarian tumors; Mucinous cyst; Pseudomyxoma peritonei
Huge Mucinous Cyst Adenoma, Case Report Series
Ali Mohammed Ali Elimam1*, Isam Mohamed Babbiker2, Reem Mohammed Elhaj Farah3, Ayat Salih Abbas4 and Omer Mohamed Abubeker Sayed5
1Assistant Professor, Department of Obstetrics and Gynecology, Elneelain University, Sudan
2Assistant Professor, Department of Obstetrics and Gynecology, University of Sinnar, Sudan
4Specialist, Obstetrics and Gynecology, Sudan
4Registrar, Obstetrics and Gynecology, Sudan
5General Practitioner, Glass Military Hospital, Sudan
*Address for Correspondence: Dr. Ali Mohammed Ali Elimam, Assistant Professor, Department of Obstetrics and Gynecology, Elneelain University, Sudan, Email: [email protected]
Mucinous cystadenoma constitutes 15% of epithelial ovarian tumors. In resource limited setting they may reach huge size as there is no regular medical checkup. This case series highlights these aspects along with diagnostic and surgical considerations.
Ovarian tumors with diameters of greater than 10 cm are referred to as giant ovarian cysts [1,2]. Among these, epithelial ovarian tumors account for 70% of ovarian tumors and commonly found in menopausal women. Nowadays these tumors are rarely seen in high income countries due to a changing behavior toward seeking medical attention and high facility set ups leading to early diagnosis and intervention. However, these tumors continue to impose a burden in developing countries and low resource setting hospitals. Generally epithelial ovarian tumors are among the most common benign ovarian neoplasms. They are thin walled, uni- or multilocular and range in size from 5 to < 20 cm. Of these, mucinous cystadenomas occur less frequently, around 15% [3-5], are more likely to be multiloculated with no surface invasion, are larger (they can attain enormous size) and are less often bilateral (less than 5%) [6].
These tumors are divided as benign, borderline and malignant accounting 80, 10 and 10% respectively, of the overall cases [7-9]. Many of these tumors are asymptomatic and found incidentally on pelvic examination or with ultrasound, especially at early stage. As the mass grow, they cause pressure symptoms, pelvic or lower abdominal pain, bloating and urinary symptoms. In addition to that rarely, patients may present with life threatening acute complications, such as ovarian torsion, cyst rupture and hemorrhage. A definitive diagnosis depends on pathologic evaluation to determine the cell type lining the cysts. Mucinous epithelial cells accumulate mucin in their cytoplasm and resemble endocervical or gastrointestinal epithelium [6]. Rarely, these mucinous lining rupture leading to, clinical syndrome characterized by diffuse mucinous peritoneal involvement, called pseudomyxoma peritonei (PMP) [10].
Mucinous tumors commonly arise from the ovary but they may arise as retroperitoneum and if not distinguished well this can cause surgical difficulties and more intraoperative complications. In small fraction of these disease, it can transform to mucinous ovarian cancer. It is a rare tumor that accounts for 3% - 4% of primary ovarian cancer [11-13].
This 70 years old obese, Para II (vaginal delivery) lady with clear medical background presented with increasing abdominal girth in the last 4years. She had been suffering from dyspeptic symptoms, vague abdominal pain and treated many times as GERD (Gastroesophageal Reflex Disorder), but with no response. Lately, the patient symptoms worsened, so she sought medical advice at the emergency department.
On physical examination: chronic sick looking, not pale or jaundiced. Vital signs all with in normal range. Clear chest, abdomen grossly distended non tender, fundal height reaching xiphoid process, with dilated superficial veins. No palpable lymph nodes. Speculum examination was normal.
Hematological and biochemical investigations were normal apart of CA125 which was 58, radiological investigations showed 40*30*18 cm Rt sided ovarian mass, elevating the diaphragm and compressing the lungs.
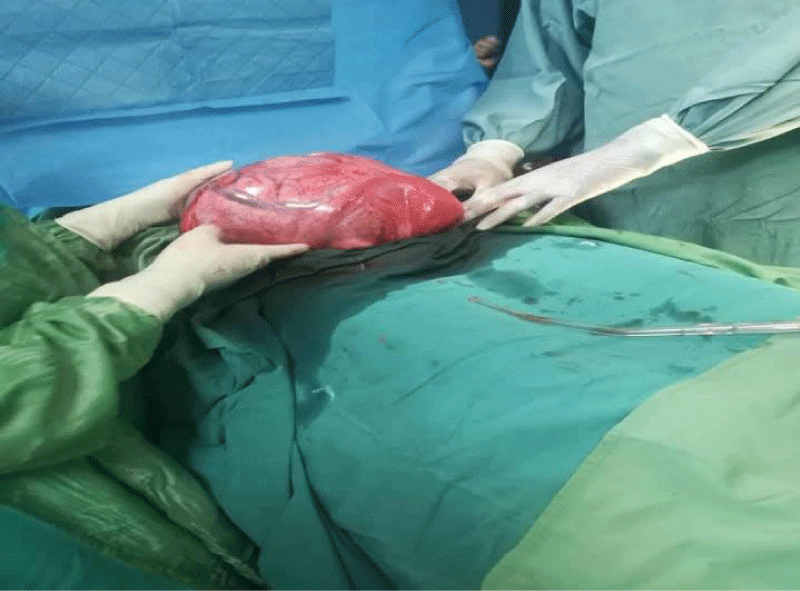
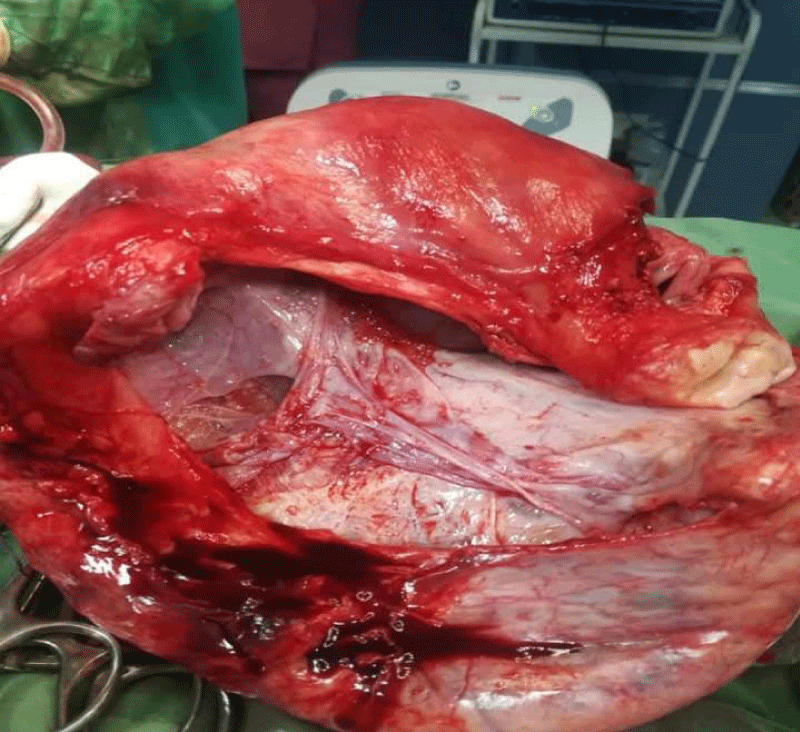
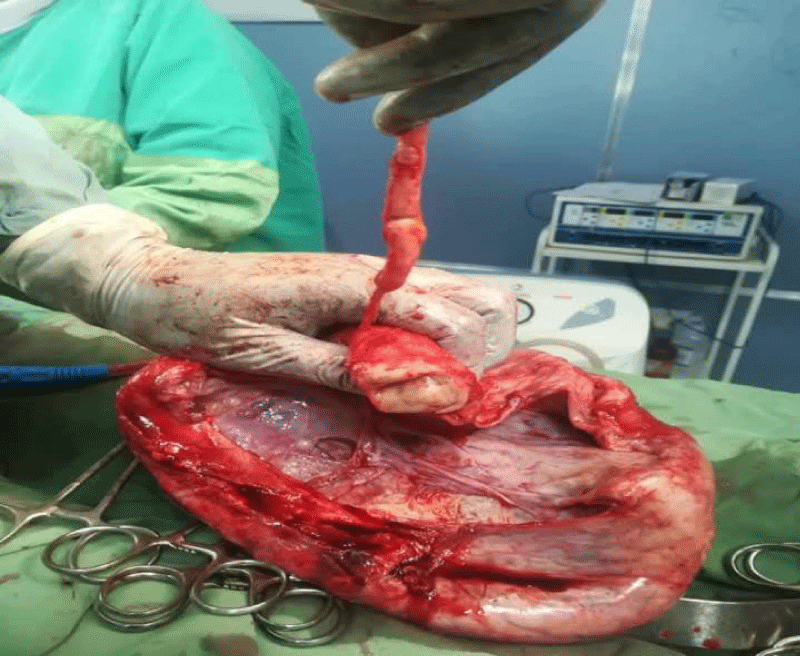
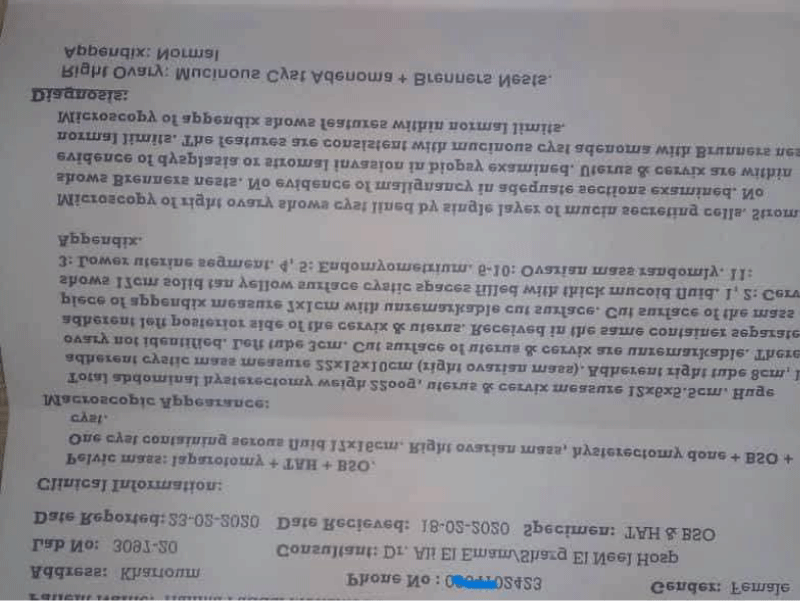
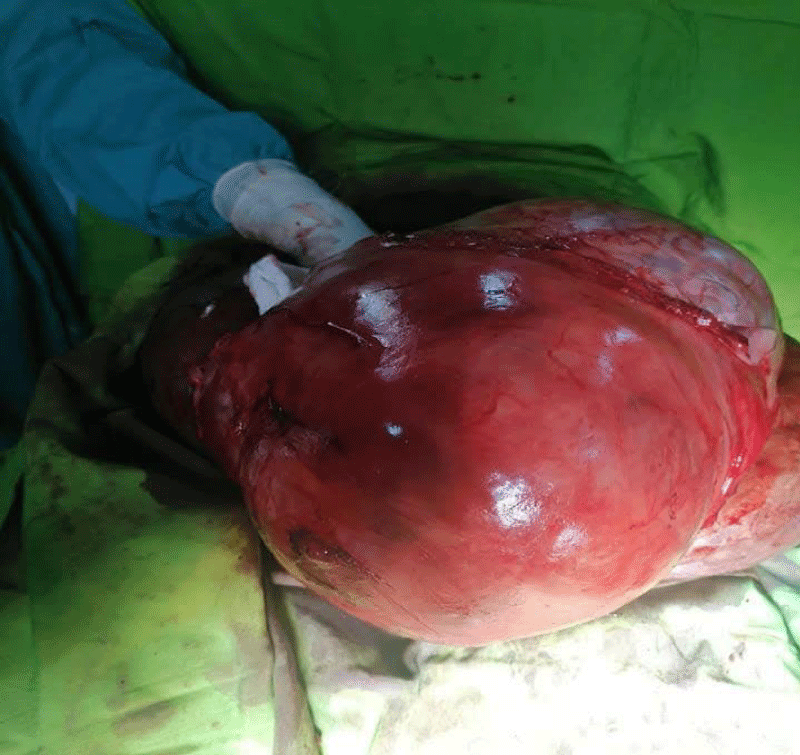
Patient stabilized and evaluated by MDT (Multi-disciplinary team) and planned for laparotomy. The operation performed under GA with left tilting to avoid aortocaval compression and hemodynamic instability. Despite extended midline incision, it was difficult to enucleate the mass intact (Picture 1), so the content drained gelatinous material (more than 12 Liters) and proceeded to total abdominal hysterectomy with bilateral salpingo-oopherectomy (TAH+BSO) and appendectomy (Pictures 2,3). Exploration of the abdominal and pelvic organs was made for possible macroscopic metastatic extensions though it was unremarkable. Histopathology confirmed mucinous cystadenoma with a normal appendix (Picture 4). The patient recovered without complications and continued follow-up in the outpatient department.
Picture 1: The huge (40*30*18 cm) cyst at starting of operation.
Picture 2: The cyst after sucking the gelatinous material.
Picture 3: The appendix, ovaries and uterus after TAH+BSO and appendectomy.
Picture 4: The histopathology report.
This 61 years old lady, Para III (vaginal delivery) with clear medical background presented with recurrent vague abdominal pain, increasing abdominal girth and occasional shortness of breath for 2 years associated with urinary and bowel symptoms. She denied any history of weight loss. The patient's symptoms gradually worsened, increasing in frequency and severity.
On examination: she was chronically sick looking with vital signs: blood pressure 120/70 mmHg, pulse rate of 85 Beats/min, respiratory rate of 21 breath/min, temperature of 36.8 oC and normal oxygen saturation. She had pink conjunctiva non icteric sclera with no palpable lymph nodes. Chest was clear and abdomen was grossly distended with no tenderness. There was a very huge mass originating from the pelvis reaching xiphisternum with visible superficial veins. Speculum examination revealed a mobile and healthy-appearing cervix.
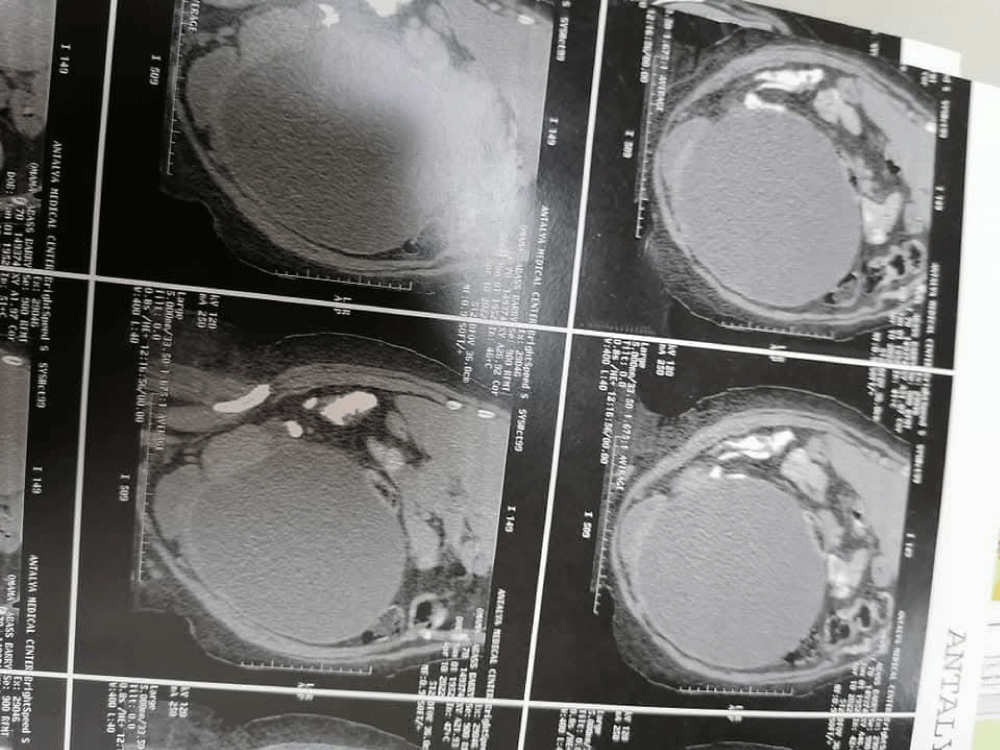
Investigations: complete blood count, urine analysis, random blood sugar, renal profile, chest radiography, CA125 all were unremarkable. Ultrasonographic scan revealed huge left sided ovarian mass with multiple septation, which was further confirmed by Computerized Tomography (CT) scan (Picture 5). No enlarged lymph nodes or ascitic fluid collection seen.
Picture 5: CT scan showing the huge cyst.
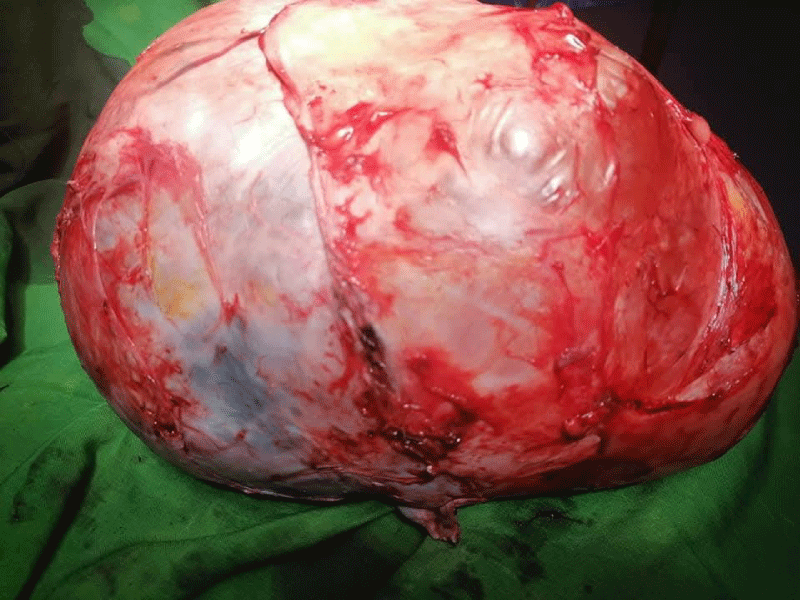
The patient received counseling and support on the provisional diagnosis, was referred to the anesthetic clinic for preoperative assessment and planned for laparotomy under General Anesthesia (GA). The ovarian mass was enucleated intact through extended midline incision (Pictures 6,7) in addition to, total abdominal hysterectomy and contralateral oopherctomy. Peritoneal wash done and it was negative for malignant cells. Exploration of the abdominal and pelvic organs was made for possible macroscopic metastatic extensions though it was unremarkable. The whole mass (Picture 7) taken without spillage for histology and revealed benign mucinous cystadenoma.
Picture 6: Huge (32*39*26 cm) cyst at the start of the operation.
Picture 7: The huge cyst enucleated intact.
Although most of mucinous ovarian tumors are benign, but they require thorough preoperative assessment and Multi-Disciplinary Team (MDT) approach to ensure good outcome. As in any ovarian mass correlation with clinical background is crucial depending on radiological, laboratory and clinical notes. Routine medical checkups and advanced imaging facilities in developed countries lead to early diagnosis and management. The absence of the attitude of routine medical checkups lead to the late presentation and worsened symptoms of both patients in our case series scenario.
Primary mucinous cystadenomas are benign commonly seen between 3rd and 6th decade [14]. The spectrum of clinical manifestation ranges from being asymptomatic to pressure symptoms. Due to the late presentation of both scenarios; they had pressure symptoms and the 2nd case worsened to the extent of bowel and urinary complaint. The most confusing point in all ovarian masses is that the presentation is vague and mimic gastrointestinal diseases in most cases (that goes with the first case scenario; who was initially managed in the medical department). MDT approach and assessment of patients by laboratory and radiological methods is important to avoid misdiagnosis and guide the treatment plan. The investigation modality of ovarian neoplasms in general is ultrasonographic evaluation followed by Computed Tomography (CT) scan or magnetic resonance imaging (MRI) along with tumor markers; final confirmation is achieved through histopathology.
The standard treatment of such ovarian mases includes total abdominal hysterectomy, bilateral salpingo-oophorectomy, peritoneal washing with or without lymphadenectomy. Histopathologic evaluation is crucial to avoid malignant transformation and to determine the need of oncologic follow up.
Mucinous cystadenoma are commonly benign masses that grow extensively, as there is no regular medical checkup in our case report series, leading to pressure symptoms. Mucinous cystadenoma can be risky if not properly managed through a Multidisciplinary Team (MDT) approach as it is associated with profound pathophysiological changes and increased morbidity. In centers with limited facility huge ovarian mass can be considered advance malignancy and surgery feared, this worsens the condition and invites further complications.
Declarations
Ethical consideration: Written informed consent was obtained for publication of personal details and accompanying images.
Data availability: All relevant data are included within the manuscript.
- Gwanzura C, Muyotcha AF, Magwali T, Chirenje ZM, Madziyire MG. Giant mucinous cystadenoma: a case report. J Med Case Rep. 2019;13(1):181. Available from: https://doi.org/10.1186/s13256-019-2102-z
- González FJA, Casares FCM, de Pedro CG, Ruiz FJP. Case of left ovarian mucinous cystadenoma, how far can it go?. J Surg. 2023;8:1731. Available from: http://www.doi.org/10.29011/2575-9760.001731
- Okafor CI, Onyegbule OA, Etigbue J, Uyoh IS, Ezenriet U. Giant mucinous cystadenoma in Nnewi, Nigeria. Ann Med Health Sci Res. 2015;5:222-225.
- Kamel RM. A massive ovarian mucinous cystadenoma: a case report. Reprod Biol Endocrinol. 2010;8:24. Available from: https://doi.org/10.1186/1477-7827-8-24
- Tola EN, Erdemoğlu E, Yalçın Y, Alkaya Solmaz F, Erdemoğlu E. A 27-kg mucinous cystadenoma of the ovary presenting with deep vein thrombosis. Turk J Obstet Gynecol. 2016;13(1):53-55. Available from: https://doi.org/10.4274/tjod.93206
- Hochberg L, Hoffman MS, Levine D, Goff B, Chakrabarti A. Adnexal mass: Differential diagnosis. UpToDate. 2023. Available from: https://www.scribd.com/document/673914754/3-Kh%E1%BB%91i-Ph%E1%BA%A7n-Ph%E1%BB%A5-Ch%E1%BA%A9n-%C4%90oan-Phan-Bi%E1%BB%87t-UpToDate
- Katke RD. A huge ovarian mucinous cystadenoma (8.5 kg) leading to bilateral hydronephrosis: a case report and review of literature. MOJ Clin Med Case Rep. 2017;7(1):166-168. Available from: https://doi.org/10.15406/mojcr.2017.07.00187
- Somagutta MR, Luvsannyam E, Jain MS, Elliott-Theberge K, Grewal AS, Pendyala SK, Edwards C. A rare case of massive ovarian mucinous cystadenoma with postmenopausal bleeding. Cureus. 2020;12(9):e10198. Available from: https://doi.org/10.7759/cureus.10198
- Katke RD. A giant case of 10 kg mucinous cystadenoma of ovary with pregnancy with previous four caesarean sections: A challenge. Int J Gynecol Reprod Sci. 2021;2(1):33–35. Available from: https://ologyjournals.com/ijgrs/ijgrs_00010.pdf
- Overman MJ, Asare EA, Compton CC. Appendix-Carcinoma. In: AJCC Cancer Staging Manual. 8th ed. Amin MB, editor. Chicago: AJCC; 2017;237.
- Hart WR, Norris HJ. Borderline and malignant mucinous tumors of the ovary: Histologic criteria and clinical behavior. Cancer. 1973;31(5):1031–45. Available from: https://doi.org/10.1002/1097-0142(197305)31:5%3C1031::aid-cncr2820310501%3E3.0.co;2-7
- Riopel MA, Ronnett BM, Kurman RJ. Evaluation of diagnostic criteria and behavior of ovarian intestinal-type mucinous tumors: atypical proliferative (borderline) tumors and intraepithelial, microinvasive, invasive, and metastatic carcinomas. Am J Surg Pathol. 1999;23(6):617–35. Available from: https://doi.org/10.1097/00000478-199906000-00001
- Hoerl HD, Hart WR. Primary ovarian mucinous cystadenocarcinomas: A clinicopathologic study of 49 cases with long-term follow-up. Am J Surg Pathol. 1998;22(12):1449–62. Available from: https://doi.org/10.1097/00000478-199812000-00002
- Preethi TP, Ranjitsingh R, Sundaram SNS, Jayaganesh P, Arcot R. Mucinous cystadenoma of ovary—how large can they grow? Sur Cas Stud Op Acc J. 2021;6:1–4. Available from: https://lupinepublishers.com/surgery-case-studies-journal/pdf/SCSOAJ.MS.ID.000240.pdf