More Information
Submitted: February 13, 2025 | Approved: March 06, 2025 | Published: March 07, 2025
How to cite this article: Fakir O, Lazhar H, Slaoui A, Lakhdar A, Baydada A. Septic Shock on Bartholinitis: Case Report and Modern Surgical Approaches. Clin J Obstet Gynecol. 2025; 8(1): 015-018. Available from:
https://dx.doi.org/10.29328/journal.cjog.1001183
DOI: 10.29328/journal.cjog.1001183
Copyright license: © 2025 Fakir O, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Abscess; Post-menopausal; Malignancy
Septic Shock on Bartholinitis: Case Report and Modern Surgical Approaches
Oumaima Fakir*, Hanaa Lazhar, Aziz Slaoui, Amina Lakhdar and Aziz Baydada
Gynaecology-Obstetrics and Endoscopy Department, Maternity Souissi, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco
*Address for Correspondence: Oumaima Fakir, Gynaecology-Obstetrics and Endoscopy Department, Maternity Souissi, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco, Email: [email protected]
Bartholinitis, or Bartholin's gland abscess, is a relatively common gynecological condition among women of reproductive age. Its annual incidence is estimated at approximately 0.5 per 1,000 women, which corresponds to a lifetime cumulative risk of about 2%. The condition primarily affects patients between 20 and 50 years old, with a peak frequency observed between 35 and 50 years.
After menopause, due to the natural involution of the gland, Bartholin's cysts and abscesses become less frequent, although they can still occur. Moreover, in women over 50, the appearance of a new mass in the gland region should prompt caution, as it may, in rare cases, indicate a carcinoma of the Bartholin's gland or an adjacent vulvar cancer. Therefore, for patients over 40 presenting with a newly emerged cyst or abscess, clinical guidelines recommend performing a biopsy or excision to rule out malignancy.
We present the case of a 50-year-old woman with no significant medical history, who was urgently referred to the gynecological emergency department due to confusion, unexplained fever of 40 °C, and resistant leucorrhoea following a week of corticosteroid antibiotic therapy. Clinical examination revealed a large, tender right vulvar mass, indicative of an acute
Bartholin's abscess. The patient exhibited signs of septic shock and was admitted to the ICU. Following a diagnosis of sepsis, broad-spectrum antibiotic therapy was initiated, alongside fluid resuscitation and norepinephrine support. Surgical drainage of the abscess confirmed the presence of E. coli. The patient's condition improved rapidly, and she was discharged on postoperative day 8 with no complications.
This case underscores that while Bartholin's abscess is typically benign, severe complications, including septic shock, can occur—especially in patients over 50. The appearance of a new Bartholin's region mass in older women should prompt consideration of malignancy, necessitating biopsy or excision. Recent studies compare various therapeutic approaches including simple incision and drainage, Word catheter placement, marsupialization, silver nitrate application, and complete gland excision. Each method has its advantages and drawbacks, with marsupialization offering lower recurrence rates and higher patient satisfaction in many instances.
Early recognition of severe infection and prompt, aggressive management combining intensive antibiotic therapy and appropriate surgical intervention is crucial to prevent life-threatening complications in Bartholin's abscess, particularly in high-risk, older patients.
Bartholinitis is an acute infection of the Bartholin's gland, often caused by bacteria such as chlamydia, gonococcus, or enterobacteria. It primarily affects young women aged 20 to 30 years. Treatment involves antibiotics and, in severe cases, surgical intervention to drain the abscess. Without treatment, bartholinitis can quickly progress to serious complications, such as a pelvi-perineal abscess or septicemia. It is therefore crucial to quickly recognize the signs of severe infection and treat it promptly to prevent these complications [1,2].
This concerns a patient aged 50, with no notable medical history, who was urgently referred by her primary care physician to the gynecological emergencies department for examination due to a state of confusion accompanied by an unexplained fever of 40 °C with chills, and suspicious leucorrhoea resistant to one week of corticosteroid antibiotic therapy.
General examination found: Glasgow Coma Scale (GCS) score of 9, fever at 40 °C, blood pressure was lower between 70/40 mmHg and 75/50 mmHg, Heart rate (tachycardia) at 130 beats per minute, and low urine output (Oliguria) < 120 ml.
A gynecological examination revealed the presence of a swollen, hardened, and tender left vulvar mass corresponding to an acute collected Bartholin's abscess (Figure 1).
Septic shock was suspected based on the patient's symptoms, and she was urgently admitted to the intensive care unit. Biologic tests showed evidence of an inflammatory response with a high white blood cell count of 30,000/mm³, CRP level at 430 mg/L, and arterial blood gas analysis revealed metabolic acidosis and hypoxemia with oxygen levels below 80 mmHg.
In response to the sepsis diagnosis and alongside the biologic tests, an urgent broad-spectrum parenteral antibiotic therapy was initiated, combining a third-generation cephalosporin and an aminoglycoside. The patient was stabilized with high-concentration oxygen therapy, a peripheral intravenous line was inserted, and fluid resuscitation was performed with crystalloids at 30 ml/kg. Additionally, norepinephrine was administered at a rate of 0.03 u/min to support blood pressure.
Further investigations were conducted to rule out other sources of infection or emergencies: a cerebral CT scan was performed due to the GCS score of 9, which came back normal; urine culture was negative; and a chest X-ray and abdominal ultrasound also showed normal results.
The patient's condition rapidly improved with fever resolution by Day 3. At 48 hours of the afebrile period, the intravenous antibiotic therapy was switched to an oral third-generation cephalosporin, and hemodynamic stability was achieved.
Surgical treatment involved incision and drainage of the abscess, obtaining a pus sample for bacterial culture, extensive washing with Dakin's solution, marsupialization, and gauze packing for 24 hours to ensure complete hemostasis. Pus samples and blood cultures were positive for E. coli.
The patient was discharged on Day 8 post-operative with a 3-week course of antibiotic therapy. During the postoperative follow-up, it was observed that the perineal wound had healed well, without any complications.
Figure 1: Folate-methionine cycle: MTHFR- methylenetetrahysrofolat; MTR- Methionine synthase; MTRR- Methionine synthase reductase; SAM-S-adenosylmethionine; SAH- S-adenosylhomocysteine; dUMP-deoxyuridinemonophsphate; dTMP- deoxyuridinemonophsphate.
Figure 2: MTHFR gene structure showing the position of C677T polymorphism in exon 4.
Epidemiology and patient profile
Bartholinitis, or Bartholin's gland abscess, is a relatively common gynecological condition in women of reproductive age. Its annual incidence is estimated at about 0.5 per 1,000 women, corresponding to a lifetime cumulative risk of approximately 2% [1]. The condition primarily affects patients between 20 and 50 years old, with a peak frequency observed between 35 and 50 years.
After menopause, due to the natural involution of the gland, Bartholin's cysts and abscesses become less common, though they can still occur. Moreover, in women over 50, the appearance of a new mass in the gland's region should prompt caution, as it may exceptionally indicate a carcinoma of the Bartholin's gland or an adjacent vulvar cancer. Therefore, for patients over 40 with a newly appeared cyst or abscess, clinical guidelines recommend performing a biopsy or excision to rule out malignancy [2,3].
Therapeutic options: marsupialization and alternatives
The primary goal in treating bartholinitis is to drain the abscess to alleviate pain and prevent the spread of infection. Several therapeutic techniques are employed, and recent studies have compared their efficacy, particularly regarding recurrence rates:
- Simple Incision and Drainage (I&D): This method, which can be performed under local anesthesia, provides rapid relief but has a high recurrence rate of up to around 40% of cases. Without additional intervention, nearly one in three patients may experience a relapse after isolated drainage [4].
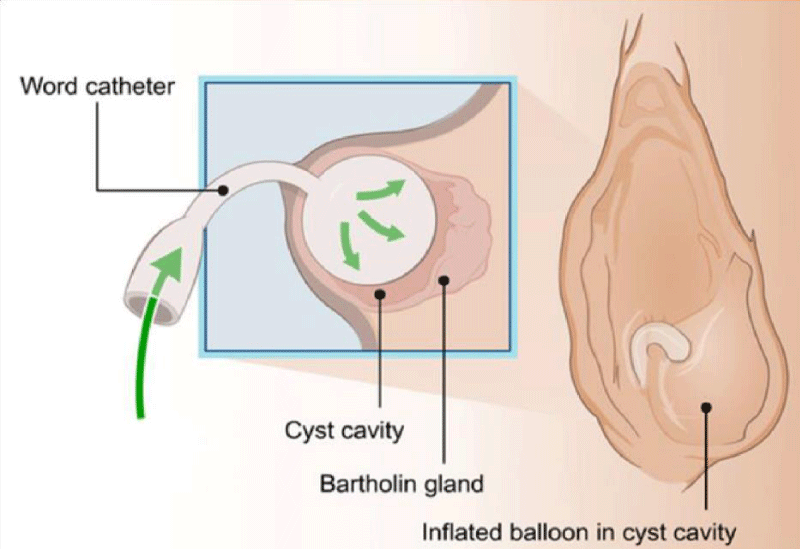
- Insertion of a Word Catheter (Prolonged Drainage) (Figure 2): Following incision, a small catheter with a balloon is inserted into the cavity and left in place for about four weeks to ensure continuous drainage and promote tract healing. This outpatient technique, which avoids general anesthesia, shows high initial healing rates, although recurrence rates of 10% to 18% have been reported [5,6]. For instance, some studies indicate a recurrence rate of 18.8% in one year with this method, highlighting that despite its simplicity and rapidity, it can be uncomfortable for some patients.
- Marsupialization: This surgical procedure involves incising the abscess and suturing the edges of the incision to the surrounding skin to create a permanent opening. Typically performed in the operating room under anesthesia, this method—although more invasive—offers superior long-term control with lower recurrence rates (between 8% and 10%) and higher patient satisfaction compared to the Word catheter. A recent retrospective study (from 2014 to 2017) reported a recurrence rate of only 8.3% after marsupialization, compared to 18.8% with the catheter (p = 0.034) [6].
- Use of silver nitrate: Less commonly used, this technique involves inserting a silver nitrate stick into the cavity after drainage to induce a chemical reaction that destroys the cyst’s epithelial lining and promotes the formation of a scar tract. A 2021 clinical study demonstrated that the addition of a silver nitrate tampon after incision resulted in a very low recurrence rate (9.1%), significantly lower than that achieved by simple incision (39.6%) or even by marsupialization (31.8%). In patients who experienced a recurrence, re-treatment with either marsupialization or silver nitrate led to healing in over 90% of cases, whereas a simple re-intervention with incision and drainage was only about 30% effective [4].
- Surgical excision of the gland: This involves the complete removal of the Bartholin's gland, a radical procedure performed under general anesthesia. It is generally reserved for cases of repeated failure of other methods or when there is suspicion of a tumor. This approach permanently eliminates the source of the problem but carries a higher risk of complications such as hemorrhage and scarring. In women over 50 presenting with refractory or atypical abscesses, some specialists prefer excision to obtain a complete histopathological examination, given the oncological risk involved. However, considering the rarity of glandular cancers, marsupialization combined with a targeted biopsy of the cyst wall may serve as an acceptable diagnostic alternative [7].
Comparison of therapeutic approaches
No single method fits all cases; the therapeutic choice depends on the clinical context and the individual characteristics of the patient. Recent data suggest that for an initial occurrence in a young woman, simple drainage followed by the placement of a catheter may be sufficient in the short term, despite a significant risk of recurrence. In contrast, for recurrences or in the presence of large abscesses, marsupialization or the use of silver nitrate yields better rates of definitive healing [4]. In postmenopausal women, due to the increased likelihood of a suspicious lesion, a more aggressive surgical approach—such as extended marsupialization or partial excision with histological analysis—is often preferred. Furthermore, older patients or those with comorbidities require closer hospital monitoring, whereas younger patients without risk factors generally tolerate outpatient treatment well.
Antibiotic protocols and microbiological etiology
Antibiotic therapy plays a crucial complementary role alongside drainage in the treatment of Bartholin's abscesses. The infectious flora is often polymicrobial, predominantly consisting of Escherichia coli and streptococci. Additionally, sexually transmitted pathogens like Neisseria gonorrhoeae may be involved in approximately 1% to 17% of cases, with Chlamydia trachomatis being less common [8,9]. Given this diversity, recommended antibiotic protocols typically cover staphylococci (including MRSA strains), streptococci, and enteric Gram-negative bacilli. Options include [5]:
- Trimethoprim-sulfamethoxazole (TMP-SMX) as monotherapy,
- The combination of amoxicillin/clavulanic acid with clindamycin,
- An alternative regimen of cefixime and clindamycin in cases of penicillin allergy.
Although drainage is the primary treatment, antibiotic therapy is particularly indicated in the presence of systemic signs (fever, chills, early sepsis), in patients with comorbidities, or when the initial treatment fails. It is also recommended to obtain a pus sample for an antibiogram to tailor the treatment accordingly [9].
Severe complications: sepsis and mortality
Fortunately, systemic complications related to Bartholin's abscess are rare. In most cases, the infection remains localized and resolves with appropriate treatment. However, without proper management, the infection can extend to surrounding tissues and, in rare cases, evolve into a fulminant infection. The literature reports a few isolated cases of Bartholin's abscess complicated by toxic shock or severe sepsis [8,10]. When the infection progresses to necrotizing fasciitis (similar to Fournier's gangrene at the vulvar level), the prognosis deteriorates significantly. This scenario is particularly concerning in patients with risk factors such as age over 50, diabetes, obesity, vascular diseases, renal insufficiency, or immunosuppression [11]. Although mortality in necrotizing fasciitis cases may reach between 13% and 50%, modern multidisciplinary management (emergency surgical debridement, resuscitation, broad-spectrum antibiotics) has reduced mortality to about 14% in some series [3]. The prognosis strongly depends on the patient’s age and comorbidities: young women generally recover better, while older or frail patients face an increased risk of multiorgan failure in the event of sepsis. In summary, an uncomplicated Bartholin's abscess does not usually threaten life, but the onset of sepsis in a vulnerable patient can have dramatic consequences. The key lies in early management with rapid drainage and intensive antibiotic therapy, supplemented by extensive debridement if necessary.
Bartholinitis is generally a benign condition but can progress to a severe form when risk factors are present, as observed in our 50-year-old patient. The therapeutic approach, which combined aggressive antibiotic therapy with surgical drainage, resulted in a favorable outcome in line with the most recent recommendations. This case underscores the importance of early recognition of signs of severity, particularly in postmenopausal patients, so that management can be promptly adapted to avoid potentially life-threatening complications.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Ethics approval and consent to participate
Ethics approval has been obtained to proceed with the current study. Written informed consent was obtained from the patient for participation in this publication.
Declarations
Guarantor of submission: The corresponding author is the guarantor of submission.
Availability of data and materials: Supporting material is available if further analysis is needed.
- Das S, Shil R, Dhanpal HN. Bartholin gland cyst and abscess: an updated scenario. International Journal of Research in Medical Sciences. 2024;12(1). Available from: https://doi.org/10.18203/2320-6012.ijrms20234030
- Kilpatrick C. Bartholin gland cyst and bartholin gland abscess [Internet]. MSD Manual Professional Edition. 2023. Available from: https://www.msdmanuals.com/professional/gynecology-and-obstetrics/miscellaneous-gynecologic-disorders/bartholin-gland-cyst-and-bartholin-gland-abscess
- Visco AG, Del Priore G. Postmenopausal bartholin gland enlargement: a hospital-based cancer risk assessment. Obstet Gynecol. 1996;87(2):286-90. Available from: https://doi.org/10.1016/0029-7844(95)00404-1
- Goklu MR, Tunc S, Andan C, Aksin S. Approach to Bartholin's abscesses and recurrences under office conditions. J Gynecol Obstet Hum Reprod. 2021;50(9):102186. Available from: https://doi.org/10.1016/j.jogoh.2021.102186
- Lee WA, Wittler M. Bartholin Gland Cyst. [Updated 2023 Jul 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532271/
- Karabük E, Ganime Aygün E. Marsupialization versus Word catheter in the treatment of Bartholin cyst or abscess: retrospective cohort study. J Turk Ger Gynecol Assoc. 2022;23(2):71-74. Available from: https://doi.org/10.4274/jtgga.galenos.2022.2022-1-6
- Wechter R, Frawley D. Postmenopausal Bartholin Gland Enlargement: Cancer Risk Assessment. Obstetrics & Gynecology. 1995;85(6):1049-1054.
- Sinha A. Management of Bartholin Gland Cyst and Abscess, Gynae Professional Forum Obstetrics and Gynaecology Directorate. S Powell Gynae SPR 10/1/2023 ver2. Available from: https://wisdom.nhs.wales/health-board-guidelines/guidelines-by-health-board/cardiff-vale/cardiff-vale-gynaecology-guidelines/bartholin-gland-cyst-abscess-management-of-cvg-guideline-2022-pdf/
- Word catheter for Bartholin’s abscess [Internet]. Chelsea and Westminster Hospital NHS Foundation Trust. Available from: https://www.chelwest.nhs.uk/your-visit/patient-leaflets/womens-services/word-catheter-for-bartholins-abscess
- Shearin RS, Boehlke J, Karanth S. Toxic shock-like syndrome associated with Bartholin's gland abscess: case report. Am J Obstet Gynecol. 1989;160(5 Pt 1):1073-4. Available from: https://doi.org/10.1016/0002-9378(89)90163-4
- Courtney-Brooks M, Scalici J, Henretta MS, Modesitt SC, Jazaeri AA, Cantrell LA, et al. Vulvar necrotizing soft tissue infection: A review of a multi-disciplinary surgical emergency and management in the modern era. Gynecol Oncol Case Rep. 2013;5:6-9. Available from: https://doi.org/10.1016/j.gynor.2013.02.002