More Information
Submitted: November 01, 2024 | Approved: November 08, 2024 | Published: November 11, 2024
How to cite this article: Lamrani M, Lakhdar K, Sardaoui S, Alami Y, Tijami F, Hachi H, et al. Fibrothecal Tumors of the Ovary - Case Report. Clin J Obstet Gynecol. 2024; 7(4): 117-119. Available from: https://dx.doi.org/10.29328/journal.cjog.1001177
DOI: 10.29328/journal.cjog.1001177
Copyright License: © 2024 Lamrani M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Fibrothecal tumors; Ovarian neoplasms; Post-Menopausal
Fibrothecal Tumors of the Ovary - Case Report
M Lamrani*, K Lakhdar, S Sardaoui, Y Alami, F Tijami, H Hachi, Z El-Hanchi and A Baydada
Department of Gynecology Obstetrics and Endoscopy, University Hospital Center Ibn Sina, Mohammed V Rabat University, Morocco
*Address for Correspondence: Meryem Lamrani, Department of Gynecology-Obstetrics and Endoscopy, University Hospital Center IBN SINA of Rabat, Mohammed V of Rabat University, Morocco, Email: [email protected]
Fibrothecal tumors of the ovary are rare neoplasms, comprising less than 4% of all ovarian tumors and primarily affecting post-menopausal women. These benign tumors arise from the stromal tissue of the ovary and may produce hormones, particularly estrogen. Their diagnosis presents considerable challenges, frequently leading to misclassification as malignant ovarian tumors or uterine myomas. This report describes the case of a 59-year-old woman who presented with abdominal distension and pelvic pain. Clinical examination revealed a large, lobulated mass and imaging studies classified the right ovarian mass as ORADS 4. An exploratory laparotomy confirmed the absence of metastasis, resulting in total hysterectomy, bilateral adnexectomy, and omentectomy. The anatomopathological analysis identified the latero-ovarian mass as a fibrothecoma. Generally, fibrothecal tumors are benign with a favorable prognosis following surgical intervention. Common symptoms include pelvic pain and abdominal distension, and diagnosis typically relies on imaging techniques such as ultrasound and CT, with definitive confirmation achieved through histopathological examination. Given their potential to mimic malignant ovarian cancer, accurate diagnosis is critical and necessitates a multidisciplinary approach.
Fibrothecal tumors of the ovary are uncommon tumors, accounting for less than 4% of all ovarian tumors [1]. They predominantly affect elderly, post-menopausal women and are characterized by their origin in the ovarian stroma, which comprises varying proportions of spindle-shaped connective cells and thecal cells [2]. Although mostly benign, these tumors can secrete hormones, primarily estrogen, potentially leading to complications such as endometrial hyperplasia. Diagnosis is complicated, as these tumors are often misidentified as uterine myomas or malignant ovarian tumors. We present the case of a 59-year-old female patient with a pelvic mass initially suggestive of advanced ovarian cancer, ultimately determined to be a fibrothecal tumor.
We present the case of a 59-year-old female with no significant medical or surgical history and no family history of cancer, nulligravida, nulliparous, and post-menopausal for 10 years. She was referred in March 2022 to the gynecological department of the National Institute of Oncology in Rabat, Morocco, for evaluation of an abdominal-pelvic mass. The patient reported increased abdominal size along with pelvic pain for three months, accompanied by anorexia, asthenia, and weight loss, without any post-menopausal metrorrhagia.
Clinical examination revealed a WHO performance status of 0, with normal cardiovascular parameters and conjunctival coloration, and no signs of androgenic activity. Abdominal examination identified an enlarged abdomen with a large, hard, mobile, lobulated mass extending to the xiphoid process. A gynecological examination via speculum showed healthy vaginal walls, while a deviated cervix was difficult to visualize. A combined vaginal and abdominal examination revealed a latero-uterine mass measuring approximately 30 cm. Rectal examination was normal, with no evidence of parametric infiltration.
Paraclinical evaluation
A pelvic ultrasound revealed a right ovarian mass with a dual solid-cystic component, measuring 26×15×10 cm and classified as ORADS 4. The left ovary was visualized, while the uterus was normal in size (6×5×4 cm) with a thickened endometrium (7 mm) and a thin layer of effusion in the pouch of Douglas. A TAP CT scan demonstrated a large tumor with cystic and solid components (26×21 cm) displacing the digestive tract, uterus, and bladder, along with effusion in the pouch of Douglas and discreet bilateral pleural effusion, but no signs of carcinosis. Laboratory results showed elevated CA-125 antigen levels (1693.60 IU/ml).
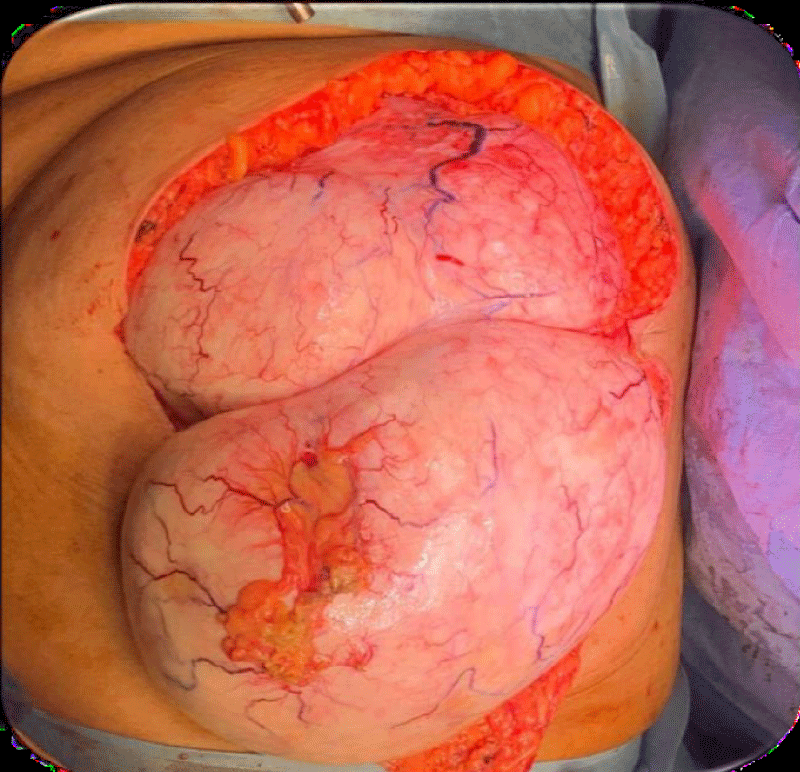
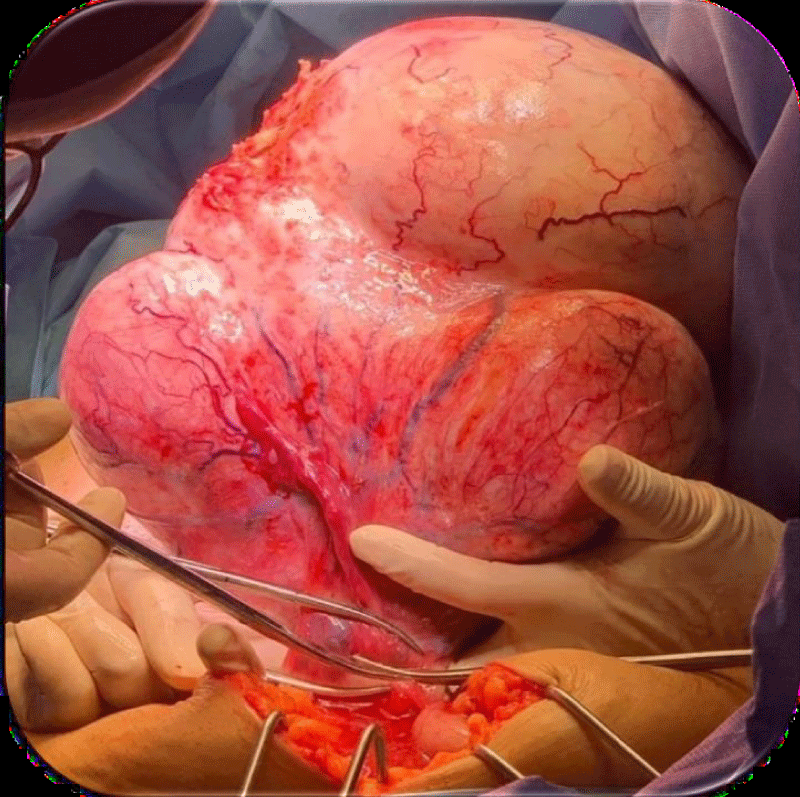
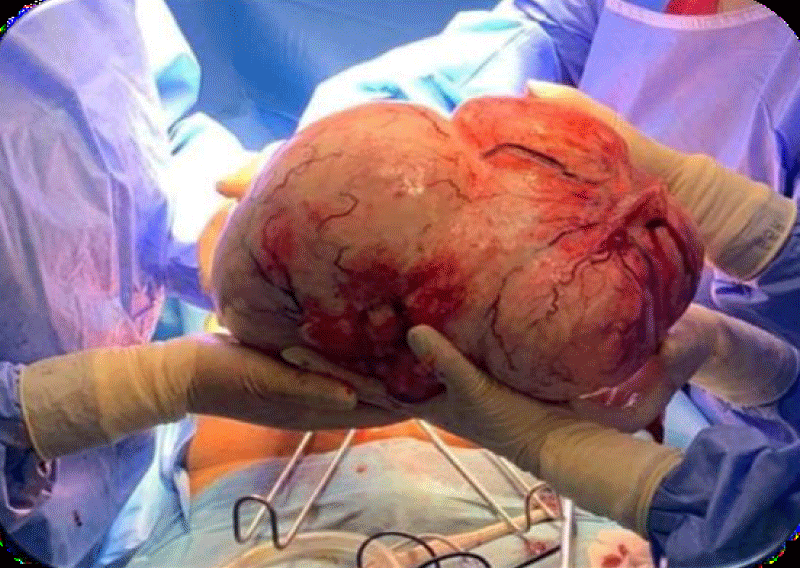
The patient underwent exploratory laparotomy, revealing no peritoneal carcinosis or liver metastases. A large right ovarian mass measuring 30 cm invaded the omentum and extended into the subhepatic region (Figures 1-3). Given the absence of metastasis, the surgical team opted for curative surgery, performing total hysterectomy with bilateral adnexectomy, appendectomy, and infra-gastric omentectomy.
Figure 1: Peroperative images of the ovarian tumor at the opening of the anterior abdominal wall.
Figure 2: Peroperative images of the ovarian tumor resection following adhesiolysis.
Figure 3: Image showing the resection of the ovarian tumor, with the surgical specimen.
Anatomopathological findings
1. Latero-ovarian mass: Identified as a fibrothecoma, characterized by fusiform cell proliferation and significant ischemic necrosis.
2. Left adnexectomy: Revealed a congested fallopian tube and a dystrophic left ovary, with no histological signs of malignancy.
3. Epiploon: Comprised fibrofatty tissue with a small leiomyoma, confirmed via immunohistochemistry.
4. Appendix: Diagnosed with non-specific chronic appendicitis.
5. Hysterectomy: The uterus exhibited a few myomas, with no histological evidence of malignancy.
After surgery, the patient was discussed at a multidisciplinary consultation meeting. Given the reassuring anatomopathological results, it was decided to continue the patient's follow-up at 1 month, 3 months, 6 months, and then 1 year. The patient's follow-up was unremarkable, with good wound healing and no signs of recurrence. She was then lost to follow-up after 1 year.
Fibrothecal tumors develop from the ovarian stroma and are predominantly benign, with malignant thecomas and fibrosarcomas accounting for less than 1% of cases [3]. These tumors generally have an excellent prognosis, with definitive cures achievable through surgical intervention. Symptoms typically include pelvic pain, abdominal distension, and, in hormone-secreting cases, metrorrhagia, which may indicate endometrial hyperplasia and warrant investigation for associated adenocarcinoma [1]. Clinically, fibrothecal tumors present as solid, mobile masses of varying sizes [3-5].
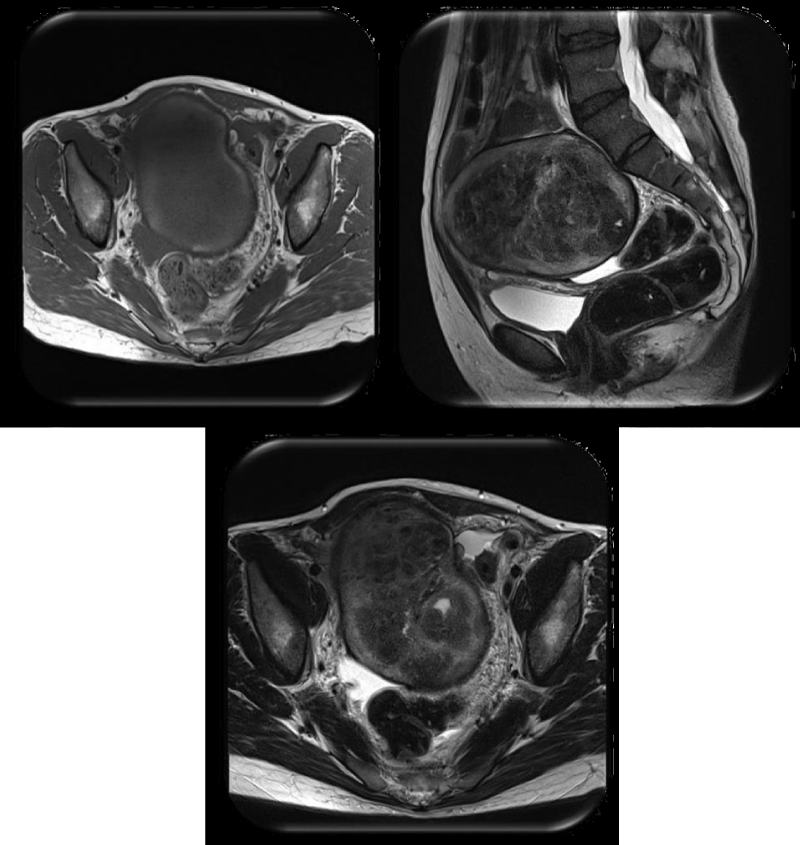
The preferred initial diagnostic imaging is pelvic ultrasound, which is non-invasive and readily available. Sonographic findings often reveal solid tumors with regular contours and homogeneous echogenicity, potentially accompanied by striated shadows. On CT, these tumors typically appear as solid masses that accumulate contrast late. MRI can identify approximately 82% of ovarian fibrothecomas, which usually present a hyposignal on T2-weighted sequences due to their fibrous composition (Figure 4) [1]. Elevated CA-125 levels often result from peritoneal irritation due to the tumor, leading to abdominal effusion [6].
Figure 4: Figure showing MRI images of ovarian fibrothecoma It shows a left-sided adnexal mass lobulated, well-circumscribed, heterogeneous, with internal fibrosis, small cystic changes, peripheral hemorrhage [7].
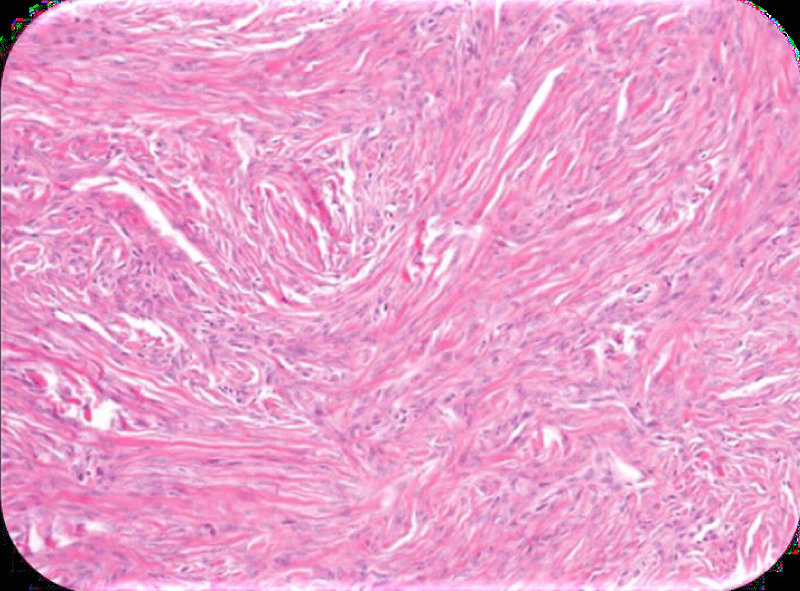
Histopathological examination remains the gold standard for diagnosis, revealing stromal tumors comprised of spindle-shaped connective cells, thecal cells, or both (Figure 5). The tumors typically appear solid, yellow, and firm [6]. Lumpectomy is the treatment of choice for younger patients, while radical surgery is reserved for peri- or post-menopausal individuals [1].
Figure 5: Figure showing the anatomopathological appearance of an ovarian fibrothecoma on slide. A Hematoxylin and Eosin (H and E) stained slide shows bland spindle cells arranged in fascicles and set within a collagenous stroma [8].
In conclusion, fibrothecal tumors are rare, benign stromal tumors primarily affecting post-menopausal women. Their presentation can easily be confused with advanced ovarian cancer, making accurate diagnosis challenging. A combination of clinical, paraclinical, and biological assessments is essential for diagnosis, with histopathological evidence serving as the definitive test. Given their potential for hormonal activity and associated complications, a thorough evaluation and a multidisciplinary approach are vital for effective management.
Declarations
Ethical approval: Ethical approval has been obtained to proceed with the current study.
Consent: Informed consent was obtained from the patient for publication of this case report and any accompanying images.
- Akharraz A, El Fazazi H, Kassidi F, Kouach J, Moussaoui D, Dehayni M. Ovarian fibrothecoma: diagnosis and treatment - About two cases. Int J Innov Sci Res. 2016;21(2):275-280. Available from: https://ijisr.issr-journals.org/abstract.php?article=IJISR-16-050-51
- Denis Q. Endocrine tumors of the ovary. In: Medico-Surgical Encyclopedia of Gynecology. Paris: Masson; 1993;680.
- Mathlouthi L, Attia Sivanesaratman V, Dutta R, Jayalakshmi P. Ovarian fibroma, clinical and histopathological characteristics. Int J Gynecol Obstet. 1990;33(3):243-247. Available from: https://doi.org/10.1016/0020-7292(90)90009-a
- Philippe E, Charpin C. Gynecological and Obstetric Pathology. Paris: Masson; 1992;196-197.
- Sfar E, Ben Ammar K, Mahjoub S, Zine S, Kchir N, Chelli H, et al. Anatomoclinical characteristics of ovarian fibrothecal tumors. A study of nineteen cases over twelve years: 1981-1992. Rev Fr Gynecol Obstet. 1994;89(5):315-321. Available from: https://www.scirp.org/reference/referencespapers?referenceid=3136105
- Slimani O, Ben Temim R, Ajroudi M, Makhlouf T, Nabil. Contribution of ultrasound in the study of fibrothecal ovarian tumors. Tunisie Medical Journal. 2017;95:469-476. Available from: https://latunisiemedicale.com/pdf/Vol%2095-01-N06.pdf
- Radswiki T, Walizai T, Ranchod A. Ovarian fibrothecoma. Radiopaedia.org. 2024. Available from: https://doi.org/10.53347/rID-14581
- Shinagare AB, Meylaerts LJ, Laury AR, Mortele KJ. MRI Features of Ovarian Fibroma and Fibrothecoma With Histopathologic Correlation. AJR Am J Roentgenol. 2012;198(3):W296-303. Available from: https://doi.org/10.2214/ajr.11.7221