More Information
Submitted: October 15, 2024 | Approved: October 17, 2024 | Published: October 18, 2024
How to cite this article: Sahay N, Aziz A, Poddar SD, Singh S. Prolonged Latency in Previable PPROM in Twin Pregnancies: A Case Series. Clin J Obstet Gynecol. 2024; 7(4): 107-111. Available from: https://dx.doi.org/10.29328/journal.cjog.1001174
DOI: 10.29328/journal.cjog.1001174
Copyright License: © 2024 Sahay N, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Dichorionic diamniotic pregnancy; Pre-viable premature rupture of membranes; Chorioamnionitis; Pulmonary hypoplasia
Prolonged Latency in Previable PPROM in Twin Pregnancies: A Case Series
Neha Sahay* , Atia Aziz, SD Poddar and Suneeta Singh
, Atia Aziz, SD Poddar and Suneeta Singh
Department of Obstetrics & Gynecology, Command Hospital, AFMC, Pune, Maharashtra, India
*Address for Correspondence: Dr. Neha Sahay, Room 23, Department of Obstetrics & Gynecology, Command Hospital, AFMC, Pune - 411040, Maharashtra, India, Email: [email protected]
Previable Preterm Premature Rupture of Membranes (PPROM) before 24 weeks of gestation in dichorionic diamniotic (DCDA) twin pregnancies is a rare and challenging obstetric complication. Three cases are presented in this case series, all involving prolonged latency periods of 74, 98, and 158 days following membrane rupture. The management strategy employed was expectant, utilizing antibiotic prophylaxis and close monitoring to prevent infection. Neonatal outcomes varied, with pulmonary hypoplasia and respiratory distress observed in some cases. One twin from Case 2 died due to sepsis, while the remaining twins in all three instances survived after extended neonatal intensive care. This series highlights the potential for extended latency and favorable outcomes in select cases, though neonatal morbidity remains a significant risk, underscoring the need for individualized counseling and vigilant care.
Previable preterm premature rupture of membranes (PPROM), defined as membrane rupture before 24 weeks of gestation, is a rare complication, occurring in less than 1% of pregnancies [1,2]. It poses significant clinical challenges for both the mother and fetus due to the increased risks of infection, preterm delivery, and neonatal morbidity and mortality. When PPROM occurs in the pre-viable period—between 14 and 24 weeks—the prognosis is often poor, with limited therapeutic options available and a high rate of pregnancy loss or extreme prematurity [3].
Previable PPROM in dichorionic diamniotic (DCDA) twin pregnancies is an even rarer event, with the incidence lower than that in singleton pregnancies. The management of such cases is particularly complex due to the unique challenges posed by the twin pregnancy, including discordant outcomes between the fetuses, increased risk of maternal complications such as infection, and higher likelihood of preterm birth [4,5]. The limited number of reported cases in the literature results in a lack of consensus regarding optimal management strategies, making clinical decision-making and counseling difficult.
In twin pregnancies complicated by PPROM, physicians must balance the potential benefits of expectant management—such as prolonging gestation and improving neonatal outcomes—against the risks of severe maternal infection (chorioamnionitis) and neonatal morbidity or mortality. Given the scarcity of evidence, prenatal counseling in cases of pre-viable PPROM in twin pregnancies is fraught with uncertainty. We report a rare case series of 3 cases of successful prolongation of PV-PPROM cases with good outcomes for fetuses. To the best of our knowledge, this is the first case series with the longest latency period from India.
Case 1
A 33-year-old woman, primigravida at 17 weeks and 3 days of gestation following IVF, presented to the labor room with complaints of watery vaginal discharge. She had no significant medical or surgical history. An abdominal ultrasound confirmed twin live DCDA intrauterine pregnancy. The scan showed a notably reduced amniotic fluid volume for fetus A, while fetus B had an adequate amniotic fluid level and normal cardiac activity was observed in both fetuses.
The patient was thoroughly counseled on the risks of miscarriage and chorioamnionitis if conservative management was chosen. She was admitted and opted for expectant management, as she had conceived via IVF after 10 years of marriage. A 5-day course of antibiotics (azithromycin 1 gram orally stat and cefotaxime 500 mg twice daily) was initiated upon admission, and the pregnancy was closely monitored for any signs of chorioamnionitis, including blood tests for total leukocyte count, procalcitonin, and C-reactive protein levels.
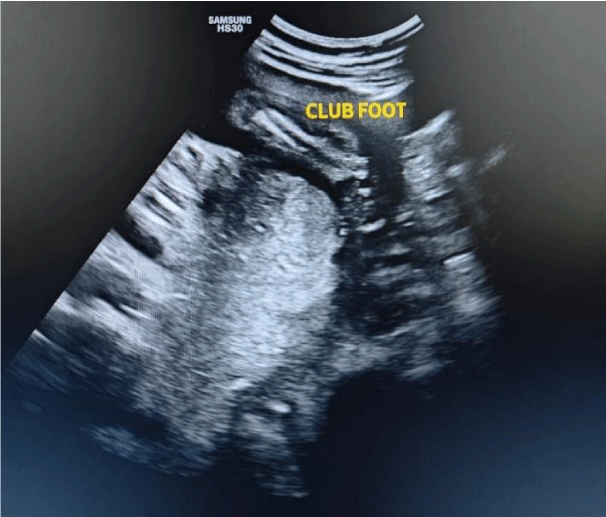
An anomaly scan at 20 weeks revealed ongoing severe oligohydramnios (deepest vertical pocket - DVP: 1.5 cm) in fetus A, along with clubfoot (Figure 1). During this period, the patient remained asymptomatic, with no abdominal pain, malodorous discharge, or signs of infection.
Figure 1: Ultrasound image of anomaly scan suggesting club foot in fetus with oligohydramnios.
At 25 weeks of gestation, the patient experienced blood-streaked vaginal fluid leakage, though there were no indications of chorioamnionitis, and her hematological parameters remained within normal limits. In anticipation of preterm delivery, a course of dexamethasone was administered. Serial ultrasounds showed that while fetus A initially demonstrated delayed growth, by 27 weeks, the growth trajectory had nearly normalized, with no apparent evidence of pulmonary hypoplasia. Notably, fetus A produced amniotic fluid, maintaining a deepest vertical pocket (DVP) of 1-1.5 cm, reassuring despite the ongoing fluid leakage.
On day 74 post-PPROM, at 28 weeks, the patient went into spontaneous preterm labor. Despite administering rescue steroids, magnesium sulfate, and tocolytics, labor progressed, and at 28w1d, a cesarean section was performed due to a preterm breech presentation of the second twin.
Twin A, a female, weighed 988 grams, with an APGAR score of 6 and 7 at 1 and 5 minutes respectively. Twin B, a male, weighed 1010 grams, with APGAR scores of 5 and 8. The placental pathology did not reveal any signs of chorioamnionitis. The mother’s postoperative recovery was smooth, and she received a 3-day course of antibiotics due to her prolonged fluid leakage.
Both twins were admitted to the neonatal intensive care unit (NICU). Twin A exhibited significant respiratory distress and retractions and was electively intubated for surfactant administration. After five days, she transitioned to nasal continuous positive airway pressure (NCPAP) for two weeks, followed by a high-flow nasal cannula for four days. Twin A was discharged after 2 months and 17 days, showing significant improvement.
Twin B was also admitted to the NICU for prematurity and respiratory distress, and treated with rescue surfactant and NCPAP, which was discontinued after two days. He was then transitioned to breastfeeding and room air. Twin B was discharged after one month with no complications and was doing well.
Case 2
A 35-year-old woman, pregnant for the first time, conceived twins through IVF after nine years of unexplained infertility. At 19 weeks of gestation, she experienced blood-tinged watery vaginal discharge and was admitted for further evaluation. Upon admission, her white blood cell count was 9,920/cumm, and her C-reactive protein (CRP) level was 1.5 mg/L. A transabdominal ultrasound confirmed a live DCDA twin pregnancy, with the DVP of amniotic fluid measuring 27 mm for twin A and 42 mm for twin B. The patient was advised to rest and was started on empirical IV antibiotics. A high vaginal swab (HVS) was collected, and she received azithromycin 1 g stat and ceftriaxone for five days.
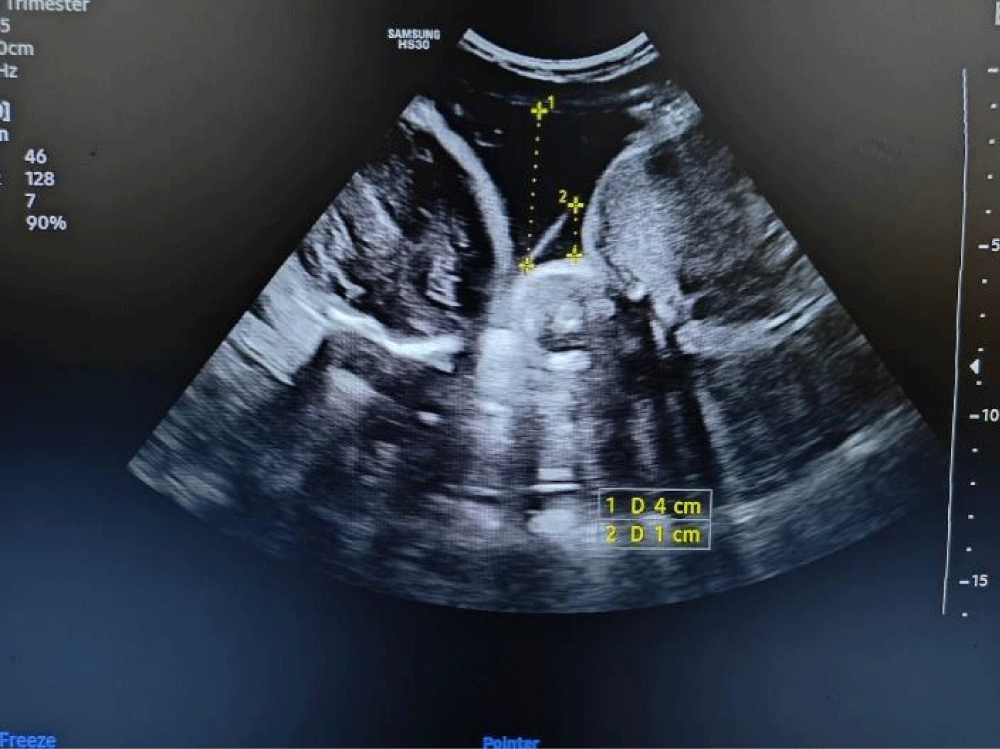
At 22 weeks of gestation, an anomaly scan revealed severe oligohydramnios in twin A, with a DVP of 1 cm, which made it difficult to detect any anomalies. In contrast, twin B had normal amniotic fluid levels (Figure 2). The patient was thoroughly counseled about potential complications, including the risk of intrauterine death of one twin, preterm labor, and maternal chorioamnionitis. Despite being informed of the risks, she was determined to continue the pregnancy. She was advised to rest and closely monitored with serial blood tests (white blood cell count, CRP), high vaginal swabs, and ultrasounds to track fetal growth and amniotic fluid levels.
Figure 2: Ultrasound image of DCDA twins showing oligohydramnios in a fetus with PROM and normal liquor in another fetus.
Throughout this time, the patient remained asymptomatic, without signs of infection such as fever, uterine tenderness, foul-smelling discharge, or abdominal pain. Follow-up ultrasounds continued to show live twins. A repeat ultrasound at 28 weeks revealed amniotic fluid of 1.8 cm DVP for twin A and 4.8 cm for twin B, though both fetuses showed adequate growth. Betamethasone was administered to promote lung development in the fetuses. The patient went into spontaneous labor at 33 weeks, 98 days after the initial episode of fluid leakage. A rescue course of steroids was given alongside tocolytics, but both babies were delivered vaginally as labor progressed.
Twin 1, a male, weighed 1.36 kg and had Apgar scores of 4 and 5 at 1 and 5 minutes, respectively. Twin 2, also male, weighed 1.6 kg with Apgar scores of 4 and 8 at 1 and 5 minutes. Both newborns were admitted to the NICU, receiving surfactant therapy and initial ventilatory support, followed by CPAP and oxygen through a nasal cannula. Sadly, twin 1 passed away 48 hours after birth due to pulmonary hypoplasia and sepsis. Twin 2 received phototherapy and CPAP for two days, then transitioned to orogastric feeding, and later breastfeeding. He maintained stable oxygen saturation on room air and was discharged 13 days after birth. Despite the hardships, the patient was able to bring home one healthy baby.
Case 3
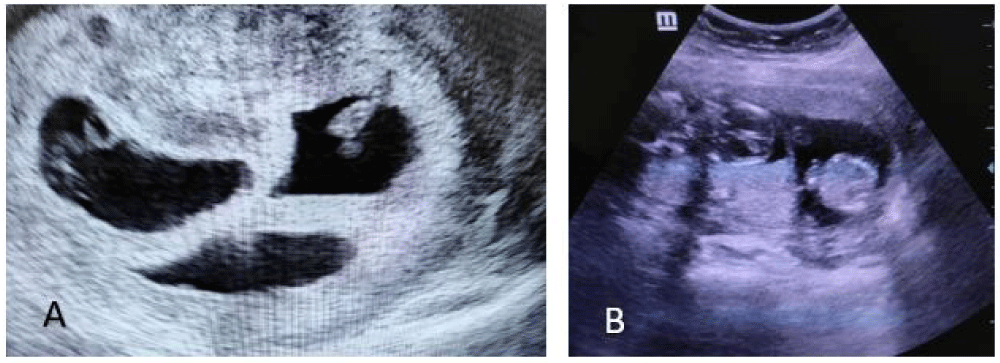
A 37-year-old woman primigravida conceived trichorionic triamniotic (TCTA) triplets following the transfer of two fresh embryos via IVF, performed due to male factor infertility. An early dating scan at seven weeks and three days of gestation confirmed the presence of three fetuses, each in separate gestational sacs (Figure 3).
Figure 3: Ultrasound image of TCTA triplet at 7 weeks POG (A) and ultrasound image after reduction of triplet to DCDA twins at 15 weeks POG (B).
The patient was counseled about the fetal and maternal risks associated with a triplet pregnancy and was offered the option of selective fetal reduction. An early structural scan at 12 weeks of gestation was unremarkable. At 13 weeks of gestation, she underwent selective fetal reduction to a diamniotic dichorionic twin pregnancy using potassium chloride (KCL) injection. However, 24 hours post-procedure, she developed leakage per vaginum from the reduced fetus, though cardiac activity in the remaining fetuses was confirmed.
The couple received extensive counseling regarding the poor prognosis associated with PPROM at such an early gestation. Despite being informed of the risks, the patient opted for conservative management. She was admitted, HVS and hematological investigations were performed, both of which were normal. After two weeks, the patient was discharged as the leakage had ceased and she remained asymptomatic.
At 20 weeks of gestation, the patient underwent an anomaly scan, which was normal for both fetuses. Four weeks later, she experienced a recurrence of leakage per vaginum, this time from one sac of the remaining twin pregnancy. She was readmitted and managed with injectable antibiotics, and inflammatory markers were assessed. A repeat ultrasound revealed a deepest vertical pocket (DVP) of 3 cm in twin 1 and 5 cm in twin 2. The leakage stopped spontaneously after one week, but due to her high-risk status for preterm delivery, the patient remained admitted.
At 28 weeks, a follow-up ultrasound showed normal amniotic fluid levels and appropriate growth of both fetuses. The patient went into spontaneous labor at 35 weeks and 4 days of gestation after 158 days of the first leaking episode. She underwent an elective cesarean section due to the breech presentation of the first twin. Twin 1, a male, weighed 2.176 kg with Apgar scores of 7 and 8 at 1 and 5 minutes, respectively. Twin 2, a female, weighed 2.332 kg with Apgar scores of 8 and 8 at 1 and 5 minutes.
Twin 1 was admitted to the NICU for 9 days and placed on continuous positive airway pressure (CPAP) due to mild respiratory distress. Twin 2 was observed in the NICU for 24 hours before being transferred to the mother's side. After two weeks, the patient was able to take both babies home.
The management of pre-viable preterm premature rupture of membranes (PPROM) in dichorionic diamniotic (DCDA) twin pregnancies presents unique challenges due to the complexities of handling twin pregnancies and the risks associated with membrane rupture before 24 weeks. The extended latency periods observed in these cases—ranging from 74 to 158 days—are notable compared to the typical one to two weeks in singleton pregnancies. This suggests that, in the absence of complications like chorioamnionitis, expectant management can significantly prolong gestation and improve neonatal outcomes. Axelson, et al. (2021) and Tandulwadkar, et al. (2024) reported cases of prolonged latency in twin pregnancies, with 114 days and 95 days, respectively, between the initial membrane rupture and delivery, both resulting in favorable outcomes for the fetuses [6,7].
A comparison with Kibel, et al. (2016) demonstrates the uniqueness of this study. Kibel’s study on PPROM in twins (between 24 – 34 weeks) found a much shorter average latency period of 5 days for twins compared to 7 days for singletons, and a higher incidence of complications like chorioamnionitis [8]. In contrast, the extended latency periods seen here, without chorioamnionitis, suggest that under the right conditions, twin pregnancies can achieve much longer gestations even after pre-viable PPROM.
Maternal infection, especially chorioamnionitis, is a significant concern with prolonged PPROM. However, none of the patients in the case series developed it, likely due to aggressive prophylactic antibiotic use and vigilant monitoring. This contrasts with Wong, et al. (2015) and Myrick, et al. (2016), both of whom reported high maternal morbidity rates, including sepsis and endometritis, following PPROM in twin pregnancies [9,10].
Neonatal outcomes were mixed, with some twins surviving after NICU care, while others faced complications such as pulmonary hypoplasia due to prolonged oligohydramnios. Pulmonary hypoplasia remains a critical factor contributing to neonatal morbidity. This is similar to Lim, et al. (2018), which found that selective reduction (SR) could prolong gestation and improve survival, with a mean latency of 120.9 days in SR cases versus 49.6 days with expectant management [11]. However, in the present cases, even without SR, extended latency was achieved, showing that expectant management can be beneficial in the absence of severe complications.
Counseling parents in these high-risk pregnancies is complex, as decisions must balance the benefits of prolonging gestation with the risks of complications like pulmonary hypoplasia and infection. These case outcomes, compared to the poorer survival rates of 43% and 27% reported by Wong and Myrick, respectively, suggest that with careful monitoring, improved outcomes can be achieved even in challenging twin pregnancies complicated by pre-viable PPROM [9,10].
The cases presented highlight the potential for successful expectant management in DCDA twin pregnancies with pre-viable PPROM. Prolonged gestation can lead to improved outcomes if complications like chorioamnionitis are prevented through careful monitoring and prophylactic treatment. The risk of neonatal morbidity, particularly from pulmonary hypoplasia, remains significant for twins with oligohydroamnios, however, the other twin is mostly unaffected if the pregnancy is prolonged and these high-risk pregnant patients can have at least one living child. Further research is needed to establish clear, evidence-based guidelines for managing these complex and high-risk cases.
Statement of ethics
Informed and written consent was taken from the couple for conservative management in all the cases. Ethical clearance is not required for this study following the local or national guidelines.
Consent to publish statement
Written informed consent was obtained from participants for publication of the details of their medical cases and any accompanying images.
Author contributions
Neha Sahay - wrote first draft of the manuscript, management of patients
Atiya Aziz, and Suneeta Singh - reviewed the manuscript, followed of the patients
S.D. Poddar - reviewed the manuscript, followed of the patient.
Data availability statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
- American College of Obstetricians and Gynecologists. Prelabor rupture of membranes: ACOG practice bulletin, number 217. Obstet Gynecol. 2020;135(0). Available from: https://doi.org/10.1097/aog.0000000000003700
- Axelson K, Osto M, Rehman R, Fakih M, Jones T. Longest survival of expectantly managed twin gestation complicated by previable preterm premature rupture of membranes at 13 weeks' gestation. Cureus. 2021;13(7). Available from: https://doi.org/10.7759/cureus.16464
- Wagner P, Sonek J, Mayr S, Abele H, Goelz R, Hoopmann M, Kagan KO. Outcome of dichorionic diamniotic twin pregnancies with spontaneous PPROM before 24 weeks' gestation. J Matern Fetal Neonatal Med. 2017;30:1750–1754. Available from: https://doi.org/10.1080/14767058.2016.1224834
- Waters TP, Mercer B. The management of preterm premature rupture of the membranes near the limit of viability. Am J Obstet Gynecol. 2009;201(3):230-240. Available from: https://doi.org/10.1016/j.ajog.2009.06.049
- Sorrenti S, Di Mascio D, Khalil A, D'Antonio F, Rizzo G, Zullo F, D'Alberti E, D'Ambrosio V, Mappa I, Muzii L, Giancotti A. Outcome of prelabor rupture of membranes before or at the limit of viability: systematic review and meta-analysis. Am J Obstet Gynecol MFM. 2024;6(6):101370. Available from: https://doi.org/10.1016/j.ajogmf.2024.101370
- Kibel M, Barrett J, Tward C, Pittini A, Kahn M, Melamed N. The natural history of preterm premature rupture of membranes in twin pregnancies. J Matern Fetal Neonatal Med. 2017;30:1829–1835. Available from: https://doi.org/10.1080/14767058.2016.1228052
- Axelson K, Osto M, Rehman R, Fakih M, Jones T. Longest survival of expectantly managed twin gestation complicated by previable preterm premature rupture of membranes at 13 weeks' gestation. Cureus. 2021;13(7). Available from: https://doi.org/10.7759/cureus.16464
- Tandulwadkar S, Mishra S, Langde S. Expectantly managed previable preterm PROM in an IVF conceived DCDA twin pregnancy: first case of longest extended latency in India. Int J Reprod Contracept Obstet Gynecol. 2024;13(3):750-752. Available from: https://doi.org/10.18203/2320-1770.ijrcog20240492
- Wong LF, Holmgren CM, Silver RM, Varner MW, Manuck TA. Outcomes of expectantly managed pregnancies with multiple gestations and preterm premature rupture of membranes prior to 26 weeks. Am J Obstet Gynecol. 2015;212:2151–2159. Available from: https://doi.org/10.1016/j.ajog.2014.09.005
- Myrick O, Dotters-Katz S, Grace M, Manuck T, Boggess K, Goodnight W. Prophylactic antibiotics in twin pregnancies complicated by previable preterm premature rupture of membranes. AJP Rep. 2016;6(3). Available from: https://doi.org/10.1055/s-0036-1587324
- Lim B, Butler B, Gagnon A, Lim K, Marquette G, Dahlgren L. Outcomes of selective reduction of DCDA twins complicated by PV-PROM compared with expectant management: a case series and review of the literature. J Obstet Gynaecol Can. 2018;40(7):919-925. Available from: https://doi.org/10.1016/j.jogc.2017.09.015