More Information
Submitted: July 31, 2023 | Approved: August 21, 2023 | Published: August 22, 2023
How to cite this article: Effendy CU, Kusika NP, Hutabarat A. Case Report: Haultain’s Method Reposition for Subacute Uterine Inversion. Clin J Obstet Gynecol. 2023; 6: 117-119.
DOI: 10.29328/journal.cjog.1001138
Copyright License: © 2023 Effendy CU, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Haultain’s method; Uterine inversion; Postpartum hemorrhage
Case Report: Haultain’s Method Reposition for Subacute Uterine Inversion
Citra Utami Effendy1*, Nicko Pisceski Kusika2 and Alwin Hutabarat3
1Resident, Department of Obstetrics and Gynecology, Faculty of Medicine, Riau University, Indonesia
2Department of Obstetrics and Gynecology, Faculty of Medicine, Riau University, Indonesia
3Department of Obstetrics and Gynecology, Dumai General Hospital, Riau University, Indonesia
*Address for Correspondence: Citra Utami Effendy, Resident, Department of Obstetrics and Gynecology, Faculty of Medicine, Riau University, Indonesia, Email: [email protected]
Background: Uterine inversion is a rare obstetric emergency but potentially life-threatening condition. If these are not immediately diagnosed, the massive and underestimated blood loss can lead to hypovolemic shock.
Case: Case of 24 years old woman was referred from the district Public Health Center with vaginal bleeding after delivery with abdominal pain. We found fundal height postpartum is 3 fingers above symphysis and confirmed a soft mass protruding inside the vagina at the local examination. The ultrasound cannot present the fundus of the uterus and impressed a uterine inversion. Stabilization for the patient is done with fluid resuscitation and blood transfusion. The patient planned for exploratory laparotomy and we confirmed uterine inversion. We did per abdominal reposition success which was managed by Haultain’s method.
Conclusion: Uterine inversion should be considered in any patient with symptoms of hemorrhage and abdominopelvic pain, with the physical findings of a soft, congested, bleeding mass within the vagina on bimanual examination. Prompt treatment consists of fluid resuscitation and anatomical repositioning is needed.
Uterine inversion is a rare obstetric emergency but potentially a serious complication of labor. This disease is characterized by severe pain and can cause life-threatening conditions. If these are not immediately identified, the massive and underestimated blood loss can lead to hypovolemic shock [1] Uterine inversion incidence varies considerably, ranging from 1 in 2,000 to 1 in 50,000 births [2]. It can be classified as acute, subacute and chronic inversion, depending on its time lag from delivery [3]. It can be acute (within 24 h of delivery), subacute (over 24 h and up to the 30th postpartum day), or chronic (> 30 days after delivery) [4].
Puerperal uterine inversion is a rare complication of the mismanaged third stage of labor in which the uterus turns inside out through the cervix. Puerperal uterine inversion is more common than non-puerperal uterine inversion and its incidence varies from 1 in 2000 to 1 in 50,000 births [1]. We feel that the Haultain procedure has not been reviewed and improved as it was used to reduce uterine inversion. This article describes a case of a uterine inversion postpartum and a review of Haultain’s procedure as the management strategy.
A 24-year-old woman referred from the Rupat Utara Public Health Center came to the Dumai General Hospital with vaginal bleeding after delivery with abdominal pain. This patient underwent Kristeller action since she delivered a 4100 grams baby. The expulsion of the placenta was smooth and normal. Following the World Health Organization’s recommendations, we performed controlled cord traction. The placenta was retracted smoothly. However, when the placenta had exited through the vagina, she starts complained of lower abdominal pain. Examination of the placenta that exited the vagina revealed incomplete cotyledon of the placenta and suspected was still left in the uterus. Active vaginal bleeding was seen. At this time, the patient developed a state of shock, exhibiting a blood pressure of 68/38 mmHg, pulse rate of 113 beats/min, and facial pallor. Stabilization for the patient is done with fluid resuscitation. The patient referred from the Rupat Utara Public Health Center came to the Dumai General Hospital with stable vital signs condition. We found fundal height postpartum is 3 fingers above symphysis and confirmed a soft mass protruding inside the vagina at the local examination. From the results of laboratory tests hemoglobin 5.4, leukocytes 11.400, platelets 542.000, and hematocrit 15%. The ultrasound cannot present the fundus of the uterus and impressed a uterine inversion.
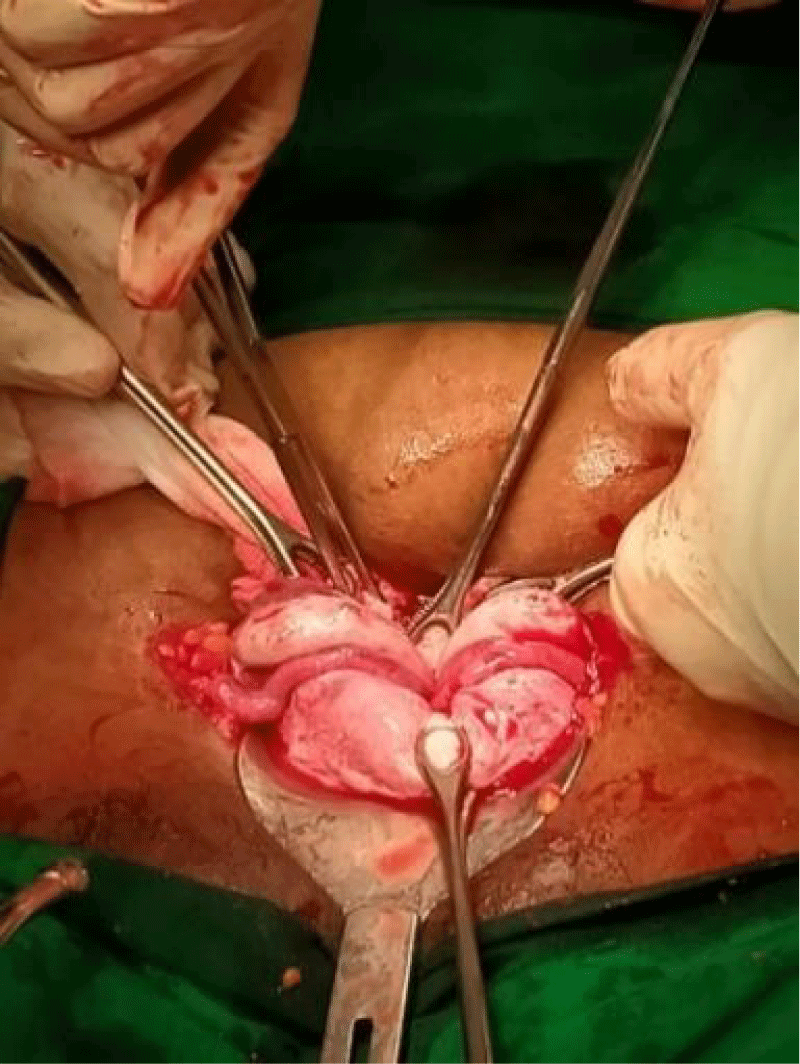
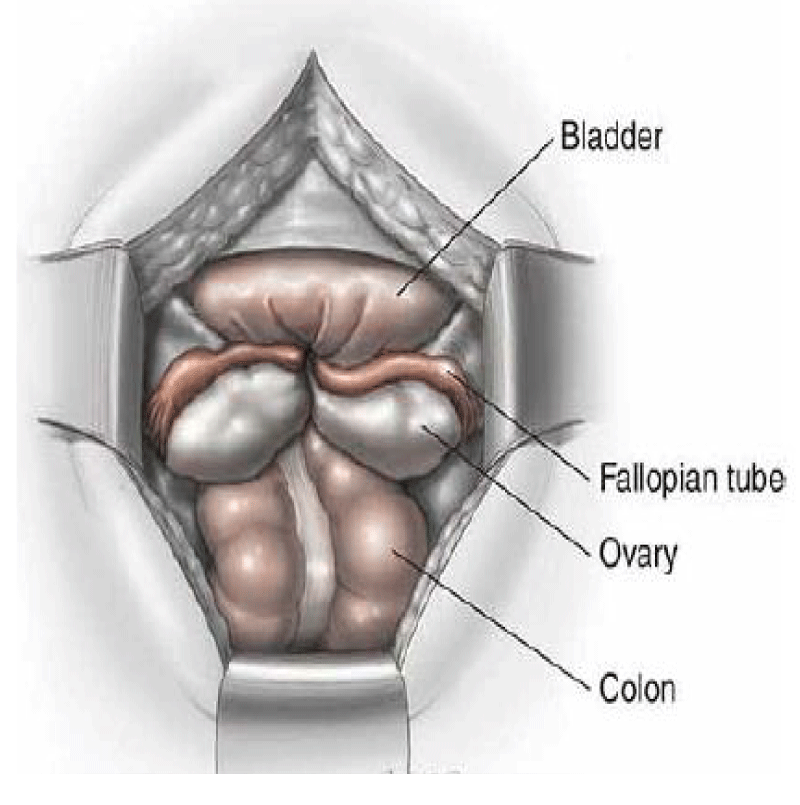
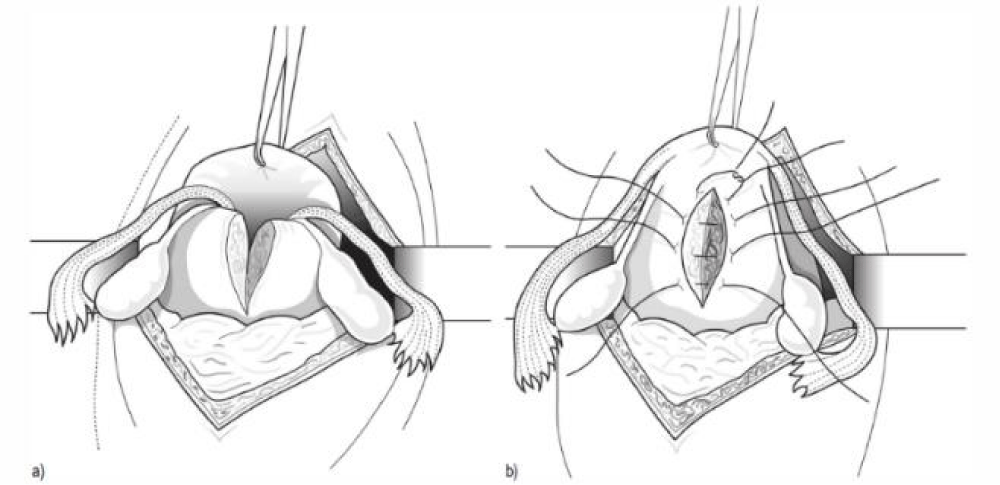
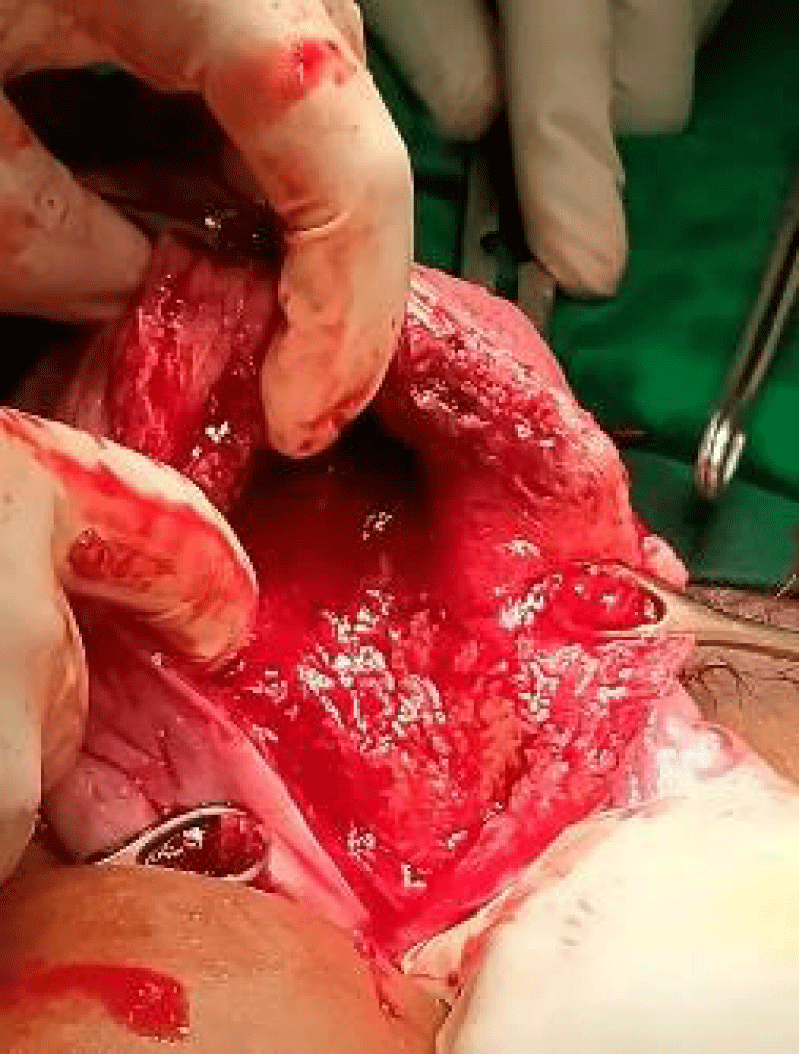
Stabilization for the patient is done with fluid resuscitation and blood transfusion. The patient didn’t plan to undergo a manual replacement attempt because it is already past 24 hours and planned to exploratory laparotomy after the hemoglobin target was achieved. In exploratory laparotomy, uterine inversion was found (Figure 1) and the depiction of uterine inversion from an abdominal perspective as explained in the textbook (Figure 2), the patient was carried out by Haultain’s procedure or uterine repositioning (Figure 3). Uterine after Haultain’s procedure of the patient (Figure 4).
Figure 1: Uterine inversion of the patient.
Graph of potassium ion concentration (Figure 2)
Figure 2: Depiction of uterine inversion from an abdominal perspective.
Graph of body weight (Figure 3)
Figure 3: Haultain’s Operation. (a) Incision of the posterior part of constricting ring. (b) Suturing uterine incision after reduction of the inversion.
Figure 4: Haultan’s Procedure of the patient.
The operation was carried out for 1 hour with 150 cc of bleeding, uterine contraction was good and there is no active vaginal bleeding.
Uterine inversion is defined as the uterine fundus turning inside out through the endometrial cavity and cervix. The causes of uterine inversion are still unexplained. Some risk factors associated with this situation are tension on the umbilical cord, fetal macrosomia, excessive fundal pressure, placenta accreta, short umbilical cord, ligament laxity, and congenital abnormalities [1]. Diagnosis is usually clinical and most patients (94%) present with significant hemorrhage, with or without shock. Shock may sometimes be neurogenic in origin owing to the excruciating pain. The differential diagnoses include a prolapsed fibroid and pelvic organ prolapse [5].
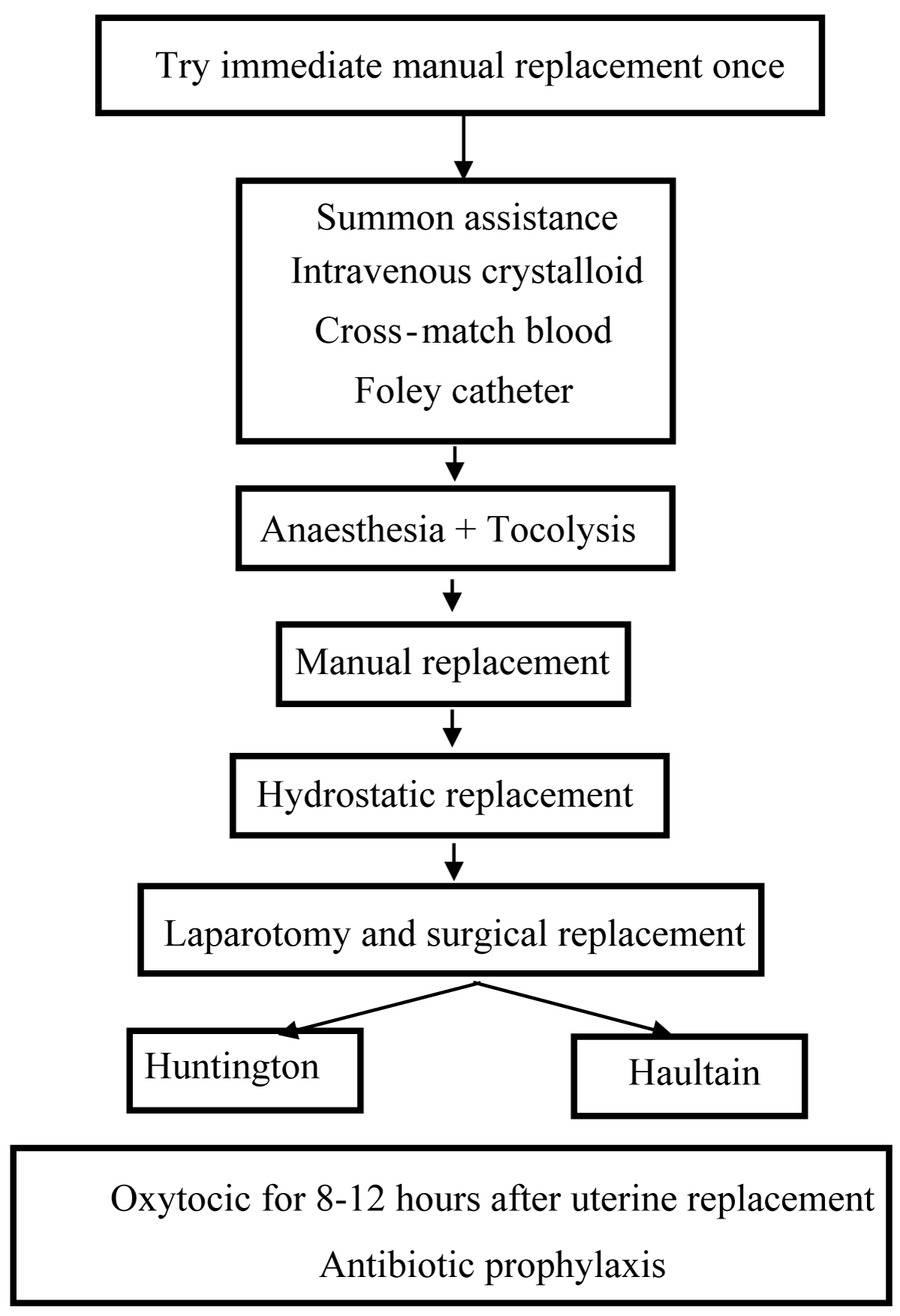
In this patient, management was performed in accordance with the Management of Acute Uterine Inversion (Figure 5) up until it was decided to perform laparotomy and surgical replacement (Haultain’s Procedure).
Figure 5: Management of acute uterine inversion [7]..
Fluid resuscitation and control of hemorrhage to restore maternal hemodynamic stability is the main goal of treatment to prevent fatal outcomes. Initial management must focus on reversing the uterus immediately [6].
Reduction of the uterus can be accomplished by several methods, both manual (nonsurgical) and surgical. In this patient, the inversion was resolved with a Haulstain’s Procedure. Antibiotic treatment has been suggested followed by hysterectomy to prevent further uterine infection [4]. Therefore, subtotal hysterectomy was considered to be more effective in the setting of hemorrhagic shock [2].
Uterine inversion is a rare and potentially life-threatening complication of pregnancy that occurs during or after the third stage of labor. There are many suggested risk factors; however, the predictability of these is unknown. Uterine inversion is a clinical diagnosis and should be considered in any patient with symptoms of hemorrhage and abdominopelvic pain, with the physical findings of a soft, congested, bleeding mass within the vagina on bimanual examination. Prompt treatment should be performed, and management of resuscitation of hypovolemia and replacement of uterine fundus to its appropriate anatomical position is needed. However, Haulstain’s procedure was performed well in this case.
Consent
Informed consent was obtained from the patient prior to the publication of this article and is available for review upon request.
- Utama BI. Chronic Uterine Inversio due to Myoma Geburt. Andalas Obstetrics and Gynecology Journal. 2020; 4(1).
- Wahono WT, Putri A, Saroyo YB, Nugroho A, Sally R. A case of third-degree hemorrhagic shock due to total subacute uterine inversion after delivery. Medical Journal of Indonesia. 2021; 30(1).
- Garg P, Bansal R. Unusual and delayed presentation of chronic uterine inversion in a young woman as a result of negligence by an untrained birth attendant: a case report. J Med Case Rep. 2020 Sep 8;14(1):143. doi: 10.1186/s13256-020-02466-x. PMID: 32895057; PMCID: PMC7487847.
- Silva BR, Meller FO, Uggioni ML, Grande JA, Silva NC. Non-Puerperal Uterine Inversion: A Systematic Review. Gynecologic and Obstetric Investigation. 2017.
- Ziki E, Madombi S, Chidakwa C, dan Zakazaka N. Reduction of subacute uterine inversion by Haultain’s method: A case report. SAJOG. 2017; 23(3).
- Sunjaya AP, Dewi AK. Total Uterine Inversion Post Partum: Case Report and Management Strategies. J Family Reprod Health. 2018 Dec;12(4):223-225. PMID: 31239851; PMCID: PMC6581659.
- Baskett TF, Calder AA, Arulkumaran S. Munro Kerrs’s Operative Obstetric. 12th Edition. London: Elsevier; 2007.