More Information
Submitted: April 08, 2022 | Approved: May 02, 2022 | Published: May 03, 2022
How to cite this article: Singh V, Paras Nath. Comparision of intra cervical PGE2 gel and transcervical Foley’s catheter for pre-induction cervical ripening. Clin J Obstet Gynecol. 2022; 5: 051-054.
DOI: 10.29328/journal.cjog.1001107
Copyright License: © 2022 Singh V, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Comparision of intra cervical PGE2 gel and transcervical Foley’s catheter for pre-induction cervical ripening
Vaishali Singh1* and Paras Nath2
1Department of Obstetrics & Gynecology, Vardhman Mahavir Medical College & Safdarjung Hospital, New Delhi, India
2Medical Officer, Siliguri District Hospital Siliguri, West Bengal, India
*Address for Correspondence: Dr. Vaishali Singh, Post Graduate Student, Presently Senior Resident, Department of Obstetrics & Gynecology, Vardhman Mahavir Medical College & Safdarjung Hospital, New Delhi, India, Email: [email protected]
Introduction: Induction of labour is a common obstetric intervention, occurring in approximately 25% of term pregnancies in developing countries. Pharmacological and mechanical methods commonly used are prostaglandin preparations (PGE1 and PGE2) and various intracervical catheters (single or double balloon), respectively.
Material and methods: Study was conducted in Siliguri District Hospital, Siliguri, Darjeeling, west Bengal. 100 antenatal woman admitted in obstetrics ward with pog more than 37 weeks were taken for study after applying inclusion and exclusion criteria. 50 were induced with cerviprime gel and 50 with intracervical foley catheter. Statistical analysis done.
Results: Mean interval between treatment initiation and delivery was not statistically significant, tachysystole was more common in group B women, rate of LSCS and NVD was similar in both groups.
Conclusion: It can be concluded from the present study that Foley’s catheter (mechanical) and prostaglandin E2 gel [pharmacological] both are effective agents for preinduction cervical ripening which substantially improve the bishops score and increase the chances of successful labour induction. There is no significant difference in their efficacy, mode of delivery and perinatal outcome.
Induction of labour is a common obstetric intervention, occurring in approximately 25% of term pregnancies in developing countries. The increased caesarean delivery risk associated with inductions strongly influenced by the induction attempt duration, especially with an unfavorable cervix [5].
Common indications for induction of labour include post-dated pregnancy, preeclampsia , and eclampsia , intrauterine fetal growth restriction, pre-labour rupture of membranes, malformed foetuses, Rh-isoimmunisation, severe hydraminos, abruptioplacenta, intrauter inefetal demisechorioamniotis, oligo hydramnios, maternal medical conditions like chronic nephritis, hypertension diabetes etc.
The contra indications to induction of labour include like previous my omectomy, previous uterine rupture, fetal transverse lie, placenta previa, vasa previa, invasive cervical cancer, active genital herpes, and previous classical or inverted T uterine incision [except inunusual circumstances such as extreme prematurity].
Pharmacological and mechanical methods commonly used are prostaglandin preparations (PGE1 and PGE2) and various intracervical catheters (single or double balloon), respectively.
Cervical ripening refers to a process of preparing the cervix for induction of labor by promoting effacement and dilatation as measured by Modified Bishop's score.
Ripening of cervix may be achieved by mechanical techniques such as introduction of trans-cervical Foleys catheter [11,12]. It can cause mechanical dilatation of cervix and stimulates endogenous release of prostaglandins by stripping the fetal membranes and release of lysosomes from decidual cells.
The study was conducted in Siliguri District Hospital, Siliguri, Darjeeling, west Bengal, for a period of one year extending from January 2018 to December 2019. It was approved by ethical committee of the institution. All the cases fulfilling the inclusion and exclusion criteria and willingness to participate in the study were included in the study and they were divided into two groups. There were total 100 cases
Inclusion criteria
- Primigravida ≥ 37 weeks of gestation
- Single ton pregnancy
- Cephalic presentation
- Bishop’s score≤ 3
- Intact membranes
- Cases where conditions were fulfilled for vaginal delivery
Exclusion criteria
- Multiple pregnancy
- Malpresentation
- Absentmembrane
- Antepartumhaemorrhage
- Previous uterinescar
- Medical diseases, e.g. heart disease, renal disease
Foley’s catheter
An 18 size Foley’s catheter (it comes in pre-sterilized pack using ethylene oxide) was introduced through cervix to extra-amniotic space using as terile technique with the aidofaspeculum and sponge holding forceps and 30 ml distilled water was instilled into the balloon. Then balloon is pulled up to the internalos. Catheter was tapped with thigh. Prophylactic antibiotic was given.
Prostaglandingel
PGE2 gel is available in the name of cerviprime gel as a sterile preparation containing 0.5 mg of dinoprostoneper 3 gm (2.5 ml) of gelinaprefilledsyringe with a catheter for endocervical application. After exposing the cervix by speculum 0.5 mg of PGE2 was inserted intra-cervically from a loaded syringe and the patients were kept in lying down position at least 30 minutes for absorption of drugs.
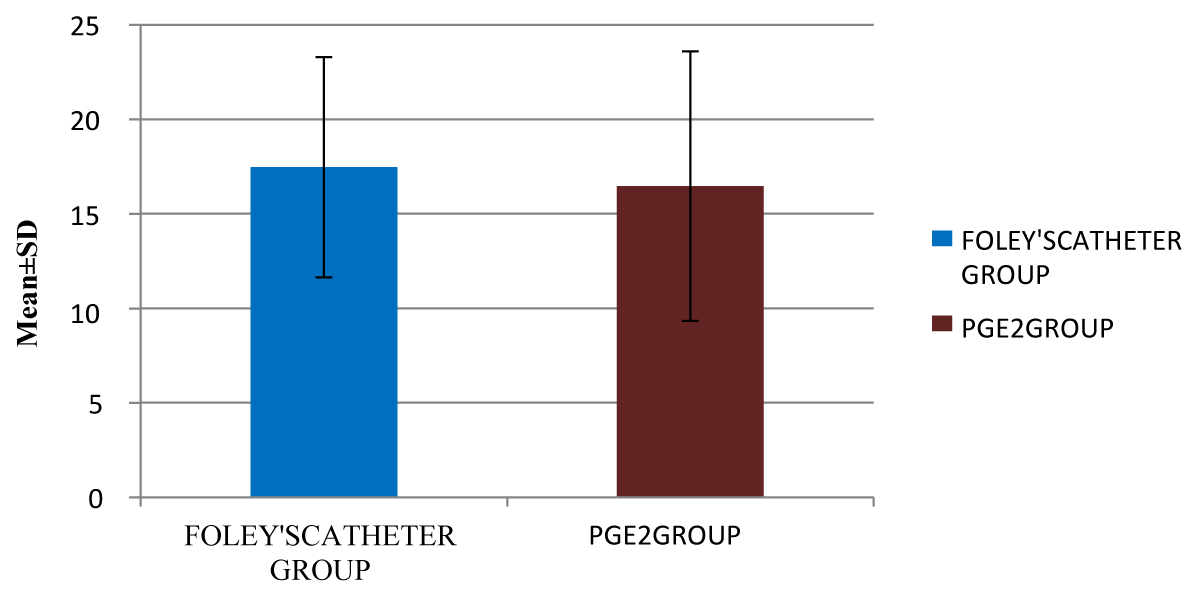
The study included 100 antenatal women attending in Siliguri District Hospital, Siliguri West Bengal, India from the period of January 2018 to December 2019, In Foley's catheter group, the mean interval between treatment initiation &delivery was 17 hrs. In PGE2 group mean interval between treatment initiation &delivery was 16 hrs. Difference of mean interval between treatment initiation & delivery between the two groups was not statistically significant (p = 0.4446) (Figure 1).
Figure 1: Mean Interval between treatment initiation and delivery (hours).
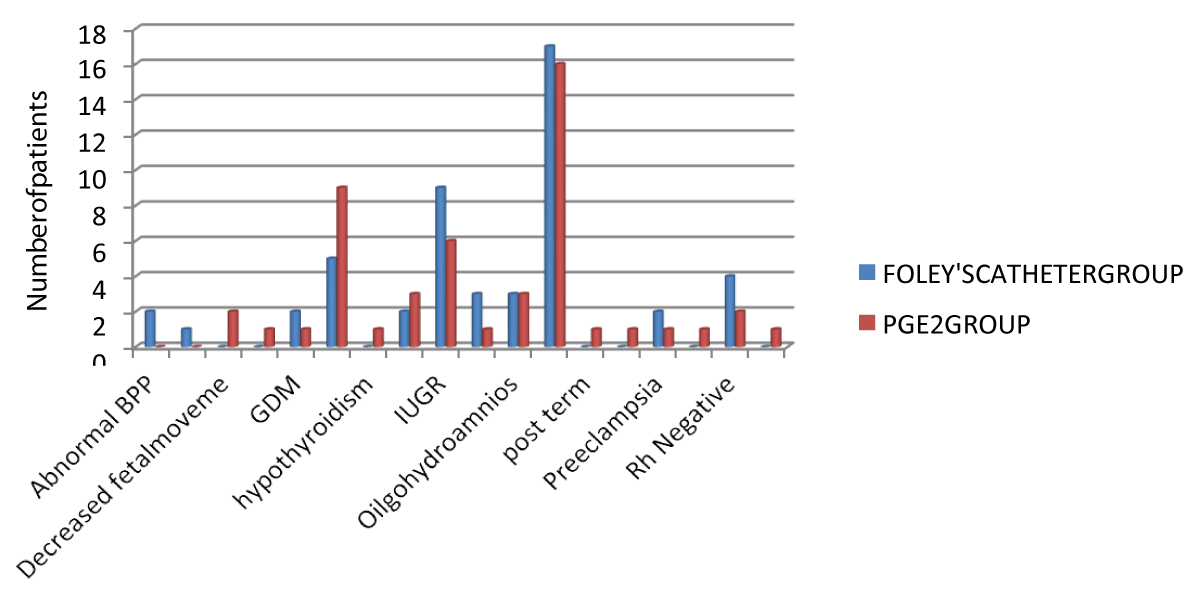
The indications were similar in the two groups, According to indication of induction, maximum number of patients 17(34.0%) were post-dated in both Foley’s catheter and PGE2 group. Association of indication of induction vs. group was not statistically significant (p = 0.5734) (Figure 2 & Table 1).
Figure 2: Mean Interval between treatment initiation and delivery (hours).
| Table 1: Maternal Complications. | ||||
| Maternal Complications | Group A | Group B | Total | p - value |
| N(%) | N(%) | |||
| NO | 46(92%) | 43(86%) | 89 | 0.65272 |
| PPH | 2(4%) | 4(8%) | 6 | 0.25014 |
| Puerperalsepsis | 1(2%) | 0(0% | 1 | 0.15854 |
| Inttrapartum pyrexia | 1(2%) | 0(0%) | 1 | 0.15854 |
| Tachysystole | 0(0%) | 3(6%) | 3 | 0.01428 |
| Total | 50 | 50 | 100 | |
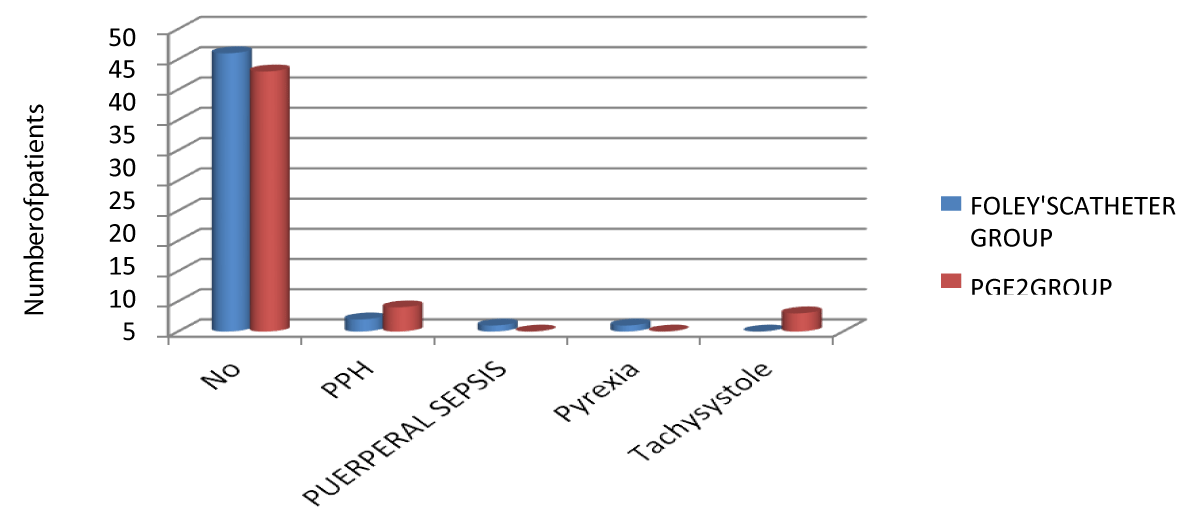
Only four patients in Group A and seven patients in Group B developed some complications. Out of these, two patients in Group A and four patients in group B had PPH. One patient in Group A and no patient in Group B developed puerperalsepsis. One patient in Group A and no patient in Group B developed intrapartum pyrexia. No patient in Group A and 3 patients in Group B developed tachysystole. Out of all these complications, only tachys to le achieved statistically significant difference (p value = 0.01428) (Figure 3).
Figure 3: Maternal complications.
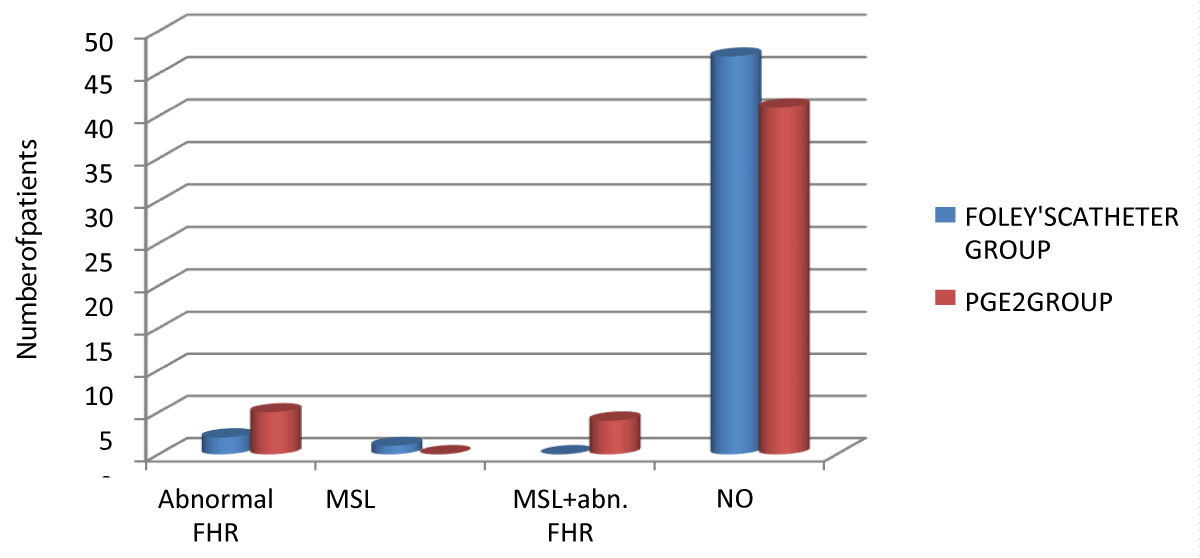
In Group A, 47(94.0%) patients had no fetal adverse effects. In Group B, 41(82.0%) had no fetal adverse effects. In group A, 2 patients had abnormal fetal heart rate whereas 5 patients in Group B had abnormal fetal heart rate. 1 patient in Group A had meconium passage whereas no patient in group B had meconium passage. Presence of both MSL and abnormal fetal heart rate was present in 4 patients in Group B. which was significantly higher compared to group B which had no patients with both MS Land abnormal FHR (p = 0.00466) (Figure 4).
Figure 4: Fetal adverse effects.
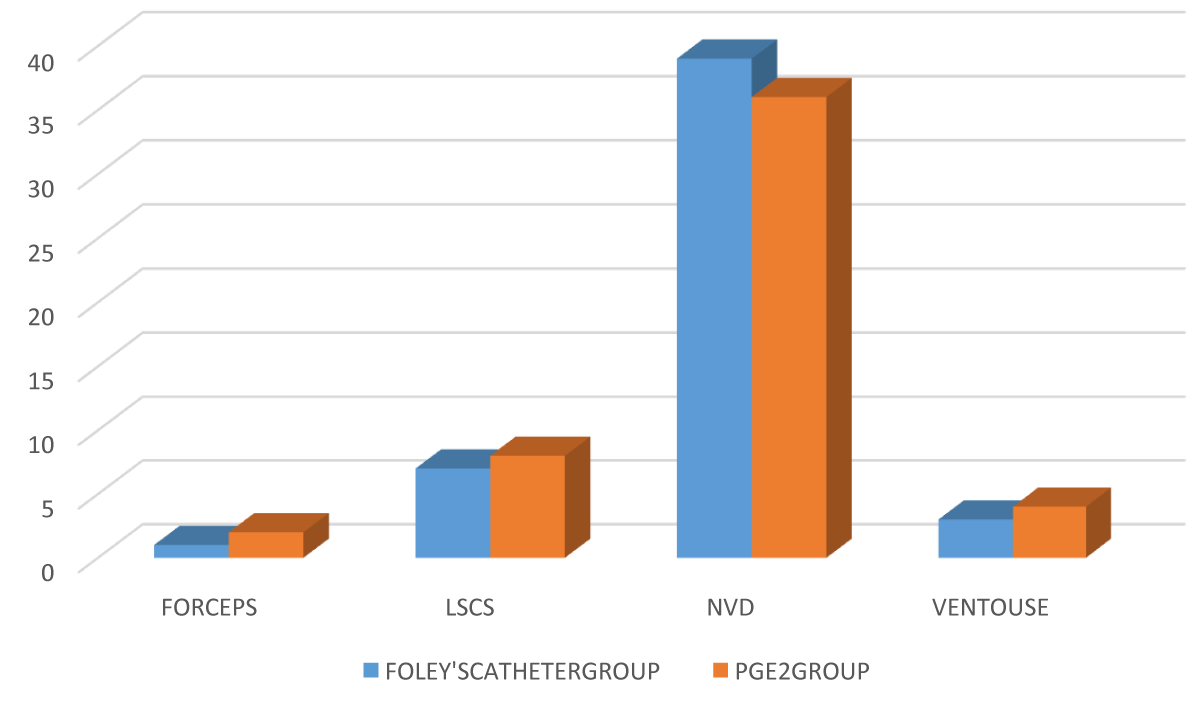
In Group A, 39 patients had normal vaginal delivery, 3 patients were delivered by ventouse and 1 patient had forceps delivery .In Group B, 36 patients had normal vaginal delivery, 4 had ventouse and 2 had forceps delivery. Rate of LSCS was 14% in Group A and 16% in Group B, The difference was not statistically significant (p = 0.3644) (Figure 5).
Figure 5: Mode of delivery.
The present study was conducted in Siliguri District Hospital, Siliguri, Darjeeling, West Bengal. 100 pregnant patients after 37 weeks gestation was randomly allocated into two groups:
Group A: Induction with extra amniotic Foley’s catheter.
Group B: Induction with intracervical PGE2 gel.
We found that in Foley's catheter group, the mean age (mean ± s.d.) of patients was 25.2200 ± 4.4414 years. In PGE2 group, the mean age (mean ± s.d) of patients was 24.5400 ± 3.7099 years. Thus age was matched in this study and difference of mean age in two was not statistically significant (p = 0.4081).
We also found that difference of mean interval between treatment initiation & delivery betweenthe two groups was not statistically significant (p = 0.4446).
We found that in Foley's catheter group, 3(6.0%) babies had NICU admission. In PGE2 group, 5(10.0%) patients had NICU admission. There was no statistically significant difference in NICU admission between the two groups (p = 0.4609).
Alam, et al. (2017) found that apgar scores, birth weights and NICU admissions showed no significant difference between the two groups. This was comparable to our study. That study shows that both Foley's catheter and PGE2 gel are equally effective in pre-induction cervical ripening.
We found that according to indication of induction, in Foley's catheter group, 17(34.0%) were postdated whereas in PGE2 group, 16(32.0%) had postdated. There was no difference between the two groups (p = 0.5734).
We found that in Foley's catheter group, higher number of patients 46(92.0%) had no maternal complications. Similarly in PGE2 group, higher number of patients 43(86.0%) had no maternal complications. Among all the maternal complications like intra partum pyrexia, tachysystole, PPH, puerperal sepsis, only tachysystole was significantly high in PGE2 group compared tofoley’s group(p = 0.0148).
Patabendige, et al. (2017) found that during induction of labour, 53(95%) reported mild or no discomfort. MBS of 6 or more was achieved in 36/56 (64%) Foley insertions. Twenty needed further intervention with prostaglandins. FC only group had 5 caesarean sections and 31 vaginal deliveries and Foley/prostaglanding roup had 7 caesarean sections and 13 vaginal deliveries.
In foley’s catheter group, 2 out of 7 patients had undergone LSCS in view of failed induction, 2 due to fetal distress and 3 due to non-progress of labour. In PGE2 group, 2 out of 8 patients had undergone LSCS in view of failed induction and 6 due to fetal distress. This difference between the two groups was not statistically significant (p = 0.2236).
Rabindranath Dalui, et al. 32found that extra amnotic Foley’s catheter balloon is an effective, safe, simple, reversible, non-pharmacological mechanical method of pre-induction cervical ripening.
It can be concluded from the present study that Foley’s catheter {mechanical} and prostaglandin E2 gel [pharmacological] both are effective agents for pre-induction cervical ripening which substantially improve the bishops score and increase the chances of successful labour induction. There is no significant difference in their efficacy, mode of delivery and perinatal outcome. The mean change in bishop’s score at 6 hours was comparable in both groups. At 12 hours improvement in bishops score was significantly more in the Foley’s catheter group. Induction of delivery interval was comparable in the two groups. Foleys catheter did not decrease the rate of caesarean section significantly but number of caesarean section done for fetal distress was less than the prostaglandin group but it was not statistically significant. Foleys catheter has fewer side effects and causes no uterine tachysystole so very strict monitoring of uterine contractions is not required during the ripening phase.
It also lacks the pharmacological side effects like vomiting and headache. Foley’s catheter causesa six fold decrease in cost as compared to PGE2 gel. Incidence of combination of meconium stained liquor and fetal distress was more in the prostaglandingroup, however NICU admission rate and mean A pgarscoreat 5 min of birth was similar in both the groups. In developing countries where cost is an important limiting factor and very stringent conditions for storage of prostagl and in may not be available, Foley’s catheter is a safe effective and relatively in expensive means of performing pre-induction cervical ripening.
- Spong CY, Berghella V, Wenstrom KD, Mercer BM, Saade GR. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop. Obstet Gynecol. 2012 Nov;120(5):1181-93. doi: 10.1097/aog.0b013e3182704880. PMID: 23090537; PMCID: PMC3548444.
- Gary CF, Kenneth LJ, Steven BL, Catherine SY, Jodi DS, Barbara HL. Williams Obstetrics. 24th Edition, Chapter 26; 2014: 525.
- Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Kirmeyer S. Births: final data for 2006. National vital statistics reports: US department of health and human services—Centers for Disease Control and Prevention.
- Alfirevic Z, Kelly AJ, Dowswell T. Intravenous oxytocin alone for cervical ripening and induction of labour. Cochrane Database Syst Rev. 2009 Oct 7;2009(4):CD003246. doi: 10.1002/14651858.CD003246.pub2. PMID: 19821304; PMCID: PMC4164045.
- Arias F, Bhide AG, Arul kumaran S, Damania K, Daftary SN, editors. Arias' Practical Guide to High-Risk Pregnancy and Delivery-E-Book: A South Asian Perspective. Elsevier Health Sciences; 2015 Jan 29.
- WorldHealthOrganization.Departmentofreproductivehealthandresearch.WHOrecommendations for induction of labour. Geneva, Switzerland: World Health Organisation; 2011:32.
- Trofatter KF Jr, Bowers D, Gall SA, Killam AP. Preinduction cervical ripening with prostaglandin E2 (Prepidil) gel. Am J Obstet Gynecol. 1985 Oct 1;153(3):268-71. doi: 10.1016/s0002-9378(85)80111-3. PMID: 3901764.
- Onge RD, Connors GT. Preinduction cervical ripening: a comparison of intracervicalprostaglandinE2gelversustheFoleycatheter.AmericanJournalofObstetrics&Gynecology.1995 Feb 1; 172(2):687-90.
- Hamilton J. Historical review of British obstetrics and gynecology. Edinburg: Livingstone; 1954; 1800-1950.
- Boulvain M, Kelly A, Lohse C, Stan C, Irion O. Mechanical methods for induction of labour. Cochrane Database Syst Rev. 2001;(4):CD001233. doi: 10.1002/14651858.CD001233. Update in: Cochrane Database Syst Rev. 2012;3:CD001233. PMID: 11687101.
- Embrey MP, Mollison BG. The unfavourable cervix and induction of labour using a cervical balloon. J Obstet Gynaecol Br Commonw. 1967 Feb;74(1):44-8. doi: 10.1111/j.1471-0528.1967.tb03931.x. PMID: 6018096.
- Obed JY, Adewole IF. The unfavourable cervix: improving the Bishop score with the Foley's catheter. West Afr J Med. 1994 Oct-Dec;13(4):209-12. PMID: 7756185.