More Information
Submitted: January 03, 2022 | Approved: January 28, 2022 | Published: January 31, 2022
How to cite this article: Nazari Z, Mortazavi L, Gordani N. Cervical choriocarcinoma in a post-menopause woman: Case report and review of literature. Clin J Obstet Gynecol. 2022; 5: 019-021.
DOI: 10.29328/journal.cjog.1001101
Copyright License: © 2022 Nazari Z, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Choriocarcinoma; Cervical polyp; Cervical neoplasm; Post-menopause
Cervical choriocarcinoma in a post-menopause woman: Case report and review of literature
Zeinab Nazari1, Leila Mortazavi2* and Noushin Gordani3
and Noushin Gordani3
1Associate Professor of Obstetrics and Gynecology, Gastrointestinal Cancer Research Center, Mazandaran University of Medical Sciences, Sari, Iran
2Assistant of Obstetrics and Gynecology, Mazandaran University of Medical Sciences, Sari, Iran
3Counseling in Midwifery, Mazandaran University of Medical Sciences, Sari, Iran
*Address for Correspondence: Dr. Leila Mortazavi, Imam Khomeini Hospital, Amir Mazandarani Blvd, Sari, Iran, Email: [email protected]
Background: Cervical choriocarcinoma is a malignant trophoblastic neoplasm that arises from pluripotent gonadal germ cells. Various manifestations are expected including vaginal bleeding and symptoms related to metastasis. Here, we report a case of primary choriocarcinoma in a post-menopausal woman.
Case presentation: A 67-year-old woman presented with vaginal bleeding and lower abdominal pain. Ultrasound and laboratory results were normal except for a β-hCG titer of 14850 IU/L. Hysteroscopy revealed a polyp in the posterior wall of the cervix. hysterectomy and bilateral salpingo-oophorectomy were performed due to suspected choriocarcinoma. The β-hCG titer decreased immediately after surgery. However, the β-hCG titer increased again one month after surgery and treatment was continued with weekly methotrexate administration.
Conclusion: Manifestations such as vaginal bleeding is very important in post-menopausal women. Although there are no specific guidelines for the treatment of choriocarcinoma in these patients, hysterectomy following chemotherapy based on response to treatment and β-hCG titration is favorable.
Cervical Choriocarcinoma is a malignant trophoblastic neoplasm that can be of gestational or non- gestational origin. The non- gestational choriocarcinoma is rare [1,2] and is more likely to develop from pluripotent gonadal germ cells in the gonads or midline structures or in association with poorly differentiated somatic carcinomas. The most common places include lung, cervix, endometrium, breast, bladder, and gastrointestinal tract [3]. The clinical diagnosis of cervical choriocarcinoma is difficult, because of its rarity and being non-specific abnormal vaginal bleeding is the most common symptom [4] and few cases of choriocarcinoma have been reported in postmenopausal women [2,5,6]. Hence, we report a case of primary cervical choriocarcinoma presented with vaginal bleeding in the post-menopausal period.
A 67-year-old female presented at the hospital with complaints of, vaginal bleeding and lower abdominal pain. She had a history of 9 vaginal deliveries and her menopause started at the age of 46. Abdominal examination was unremarkable. Abdominal and pelvic ultrasound reported normal ovaries, normal uterus with the size of 110 x 48 x 37 mm and uterine thickness of 12 mm. Primary laboratory tests showed a hemoglobin of 12.7 mg/dL, platelets count of 96000/micL, prothrombin time (PT) of 16.8 sec, partial thromboplastin time (PTT) of 30 sec, and INR of 1.2. Further laboratory tests revealed a β-hCG titer of 14850 IU/L. The next day, β-hCG titer reached 7100 IU/L. CA 19-9, CA 125, CA 15-3, and CEA markers were negative. A chest CT scan displayed no findings regarding metastasis. Hysteroscopy was performed on the patient and a polyp was observed in the posterior wall of the cervix. She underwent surgery for a Total Abdominal Hysterectomy and Bilateral Salpingo-Oophorectomy (TAH-BSO).
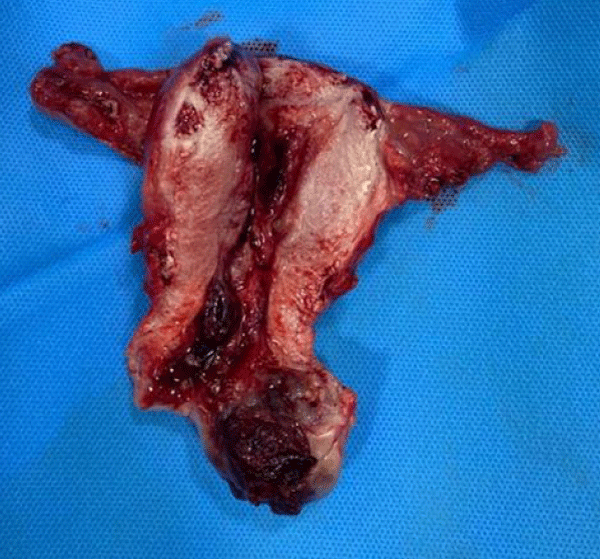
In the operating room, the patient was placed in the supine position. After induction of anesthesia and endotracheal intubation, a Pfannenstiel incision was made to reach the pelvic cavity. Abdominal and pelvic cavities were explored for metastasis. A hemorrhagic lesion with the size of 40 x 38 mm was observed in the posterior wall of the cervix. The lesion was extended to the uterine cavity. Further, total hysterectomy and bilateral Salpingo-oophorectomy was performed. After hemostasis, the abdomen was closed.
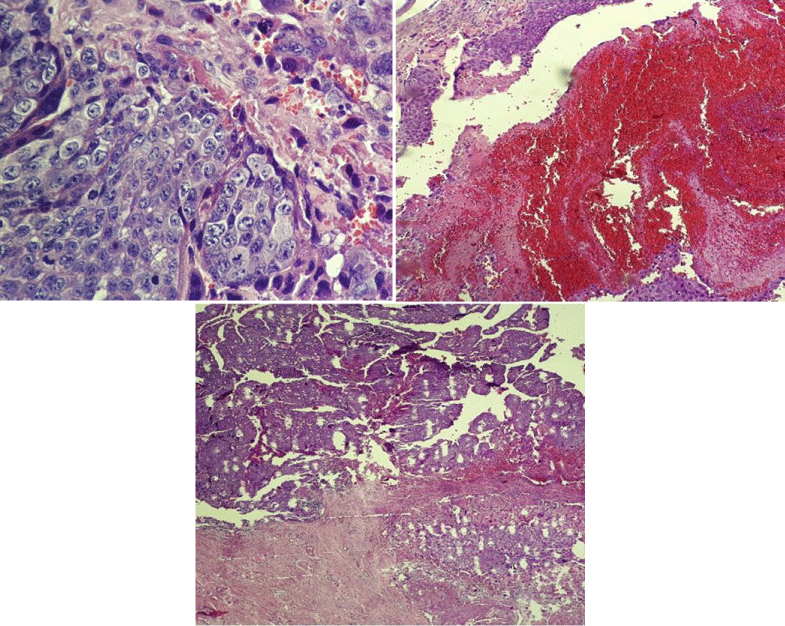
The pathological study of the lesion reported endocervical polyp invasion, along with hemorrhage and necrosis. Biphasic appearance of mononuclear cytotrophoblasts and multinucleated syncytiotrophoblasts was observed with hemorrhage. There was no peritoneal and intra-lymphatic invasion. Uterine corpus and adnexa were spared. Endometrial hyperplastic polyp was also reported in the lower segment of the uterus (Figure 1). Pathological images are shown in Figure 2.
Figure 1: Primary lesion of the cervix with the size of 40 x 38 mm invading the uterine cavity.
Figure 2: Histological images of choriocarcinoma (A Collection of Surgical Pathology Images).
Serial evaluation of β-hCG on days 7 and 14 post-operatively showed the titers of 1006 IU/L, and 371 IU/L, respectively. In addition, on the 30th day after surgery, the β-hCG titer reached 136 IU/L. However, a week later the β-hCG titer rose to 179 IU/L. It was decided to prescribe methotrexate to prevent tumor recurrence. 110 mg of methotrexate was administered intravenously each for the next 4 weeks. After the final dose of methotrexate is 110 mg, the titer of β-hCG was less than 2 IU/L (Table 1). Subsequently, the patient underwent monthly examination and β-hCG titer evaluation. Vaginal examination was normal.
| Table 1: β-hCG titer changes during treatment. | |
| Measurement time | β-hCG values |
| Before surgery | 14850 |
| 2th after surgery | 7100 |
| 7th day after surgery | 1006 |
| 14th day after surgery | 371 |
| 30th day after surgery | 136 |
| 37th day after surgery | 179 |
| 65th day after surgery and 30th days after starting methotrexate | 2 |
| 95th days after surgery and 60th days after starting methotrexate | Negative |
| 125th days after surgery and 90th days after starting methotrexate | Negative |
Gestational choriocarcinoma (GCC) is a tumor in women of reproductive age with a history of previous miscarriage or molar or ectopic pregnancy [2]. Non-gestational choriocarcinoma (NGCC) is a very rare subtype of choriocarcinoma differing in origin and phenotypic characteristics compared to (GCC), it is not linked to any form of pregnancy [7] one of the symptoms of (NGCC) is persistent or irregular vaginal bleeding [8], which is life-threatening [9] and massive bleeding due to its rapid growth is considered an emergency. Metastasis may occur in the lungs, pelvis and vagina. Rare sites include the gastrointestinal tract, spleen and kidneys. The central nervous system is rarely involved in the absence of pulmonary metastasis [8]. Differentiation of gestational choriocarcinoma from non-gestational type is usually obtained by DNA polymorphism analysis. Histopathological studies alone are not able to distinguish between these two types unless there is evidence of a previous pregnancy or a history of other germ cell tumors [10].
Treatment of cervical choriocarcinoma is a combination of hysterectomy and chemotherapy. Cerebral metastasis is reported in 8% - 15% of gestational trophoblastic neoplasms. In these cases, treatment is based on a combination of radiation therapy and chemotherapy to stabilize the patient. However, surgical interventions such as craniotomy may be needed to prevent neurological deterioration due to cerebral hemorrhage [11]. Although there are no specific guidelines for the treatment of choriocarcinoma in post-menopausal patients, there are some evidences regarding the efficacy of etoposide, methotrexate, actinomycin-D, cyclophosphamide and vincristine (EMA-CO regimen) as first-line treatment of metastatic high-risk gestational trophoblastic neoplasia [12]. Manifestations such as vaginal bleeding are very important in post-menopausal women. The workup showed no evidence of metastasis to our patient. Based on high initial β-hCG titers, abdominal hysterectomy was considered for the patient. Although the β-hCG titer decreased immediately after surgery, it was decided to continue treatment with methotrexate due to the re-increase of the β-hCG titer. This patient had a history of multiple vaginal deliveries with a very rare type of neoplasm that had an unusual manifestation and was well treated with a combination of hysterectomy and methotrexate.
Declarations
Statement of ethics: Consent from the patient was obtained for this publication.
Conflicts of interest: The authors declare that they have no conflicts of interest.
- Mangla M, Singla D, Kaur H, Sharma S. Unusual clinical presentations of choriocarcinoma: A systematic review of case reports. Taiwan J Obstet Gynecol. 2017; 56: 1-8. PubMed: https://pubmed.ncbi.nlm.nih.gov/28254207/
- Joshi SM, Das T, Dagar M, Srivastava M, Ganguli I, et al. A Rare Case of Choriocarcinoma. IJOPARB. 2020: 33.
- Stockton L, Green E, Kaur B, De Winton E. Non-gestational choriocarcinoma with widespread metastases presenting with type 1 respiratory failure in a 39-year-old female: case report and review of the literature. Case Rep Oncol. 2018; 11: 151-158. PubMed: https://pubmed.ncbi.nlm.nih.gov/29681814/
- Sorbi F, Sisti G, Pieralli A, Di Tommaso M, Livi L, et al. Cervicoisthmic choriocarcinoma mimicking cesarean section scar ectopic pregnancy. J Res Med Sci. 2013; 18: 914-917. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3897080/
- Desai NR, Gupta S, Said R, Desai P, Dai Q. Choriocarcinoma in a 73-year-old woman: a case report and review of the literature. J Med Case Rep. 2010; 4: 379. PubMed: https://pubmed.ncbi.nlm.nih.gov/21108779/
- Guo N, Yin R, Li Q, Song L, Wang D. Postmenopausal choriocarcinoma: a rare case report and review of the literature. Menopause. 2018; 25: 239-241. PubMed: https://pubmed.ncbi.nlm.nih.gov/28816932/
- Lazare C, Zhi W, Dai J, Cao C, Sookha RR, et al. A pilot study comparing the genetic molecular biology of gestational and non-gestational choriocarcinoma. Am J Transl Res. 2019; 11: 7049-7062. PubMed: https://pubmed.ncbi.nlm.nih.gov/31814908/
- Balagopal P, Pandey M, Chandramohan K, Somanathan T, Kumar A. Unusual presentation of choriocarcinoma. World J Surg Oncol. 2003; 1: 1-4. PubMed: https://pubmed.ncbi.nlm.nih.gov/12773221/
- Chandacham A, Kietpeerakool C, Khunamornpong S, Suprasert P, Srisomboon J, et al. Successfully conservative treatment of large cervical choriocarcinoma with profuse vaginal bleeding. J Med Assoc Thai. 2009; 92: 120-123. PubMed: https://pubmed.ncbi.nlm.nih.gov/19260253/
- Tsujioka H, Hamada H, Miyakawa T, Hachisuga T, Kawarabayashi T. A pure nongestational choriocarcinoma of the ovary diagnosed with DNA polymorphism analysis. Gynecol Oncol. 2003; 89: 540-542. PubMed: https://pubmed.ncbi.nlm.nih.gov/12798727/
- Doll KM, Soper JT. The role of surgery in the management of gestational trophoblastic neoplasia. Obstet Gynecol Surv. 2013; 68: 533-542. PubMed: https://pubmed.ncbi.nlm.nih.gov/23803756/
- Goldfarb JA, Dinoi G, Mariani A, Langstraat CL. A case of multi-agent drug resistant choriocarcinoma treated with Pembrolizumab. Gynecol Oncol Rep. 2020; 32: 100574. PubMed: https://pubmed.ncbi.nlm.nih.gov/32395603/