More Information
Submitted: December 21, 2021 | Approved: January 17, 2022 | Published: January 18, 2022
How to cite this article: Crowley CM, Gill N, Geisler M. Outpatient operative hysteroscopy: evaluation of patient satisfaction and acceptance. Clin J Obstet Gynecol. 2022; 5: 005-008.
DOI: 10.29328/journal.cjog.1001098
Copyright License: © 2022 Crowley CM, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Outpatient operative hysteroscopy: evaluation of patient satisfaction and acceptance
Clare Margaret Crowley*, Noelle Gill and Minna Geisler
Department of Obstetrics and Gynaecology, CCork University Hospital, Maternity Hospital, Wilton, Cork, Ireland
*Address for Correspondence: Clare Margaret Crowley, Department of Obstetrics and Gynaecology, Cork University Hospital, Maternity Hospital, Wilton, Cork, Ireland, Email: [email protected]
Aims: To examine patient satisfaction of an outpatient operative hysteroscopy performed by both doctors and nurse hysteroscopists. Secondly, compare satisfaction, complications, and failure rate of these procedures performed by doctors and nurse hysteroscopists.
Methods: In this retrospective study, the charts of 80 women who attended the service over one year were examined. Women were included if either an endometrial polyp or submucosal leiomyoma required removal using an endoscopic morcellator. All women had signed a consent form for the procedure.
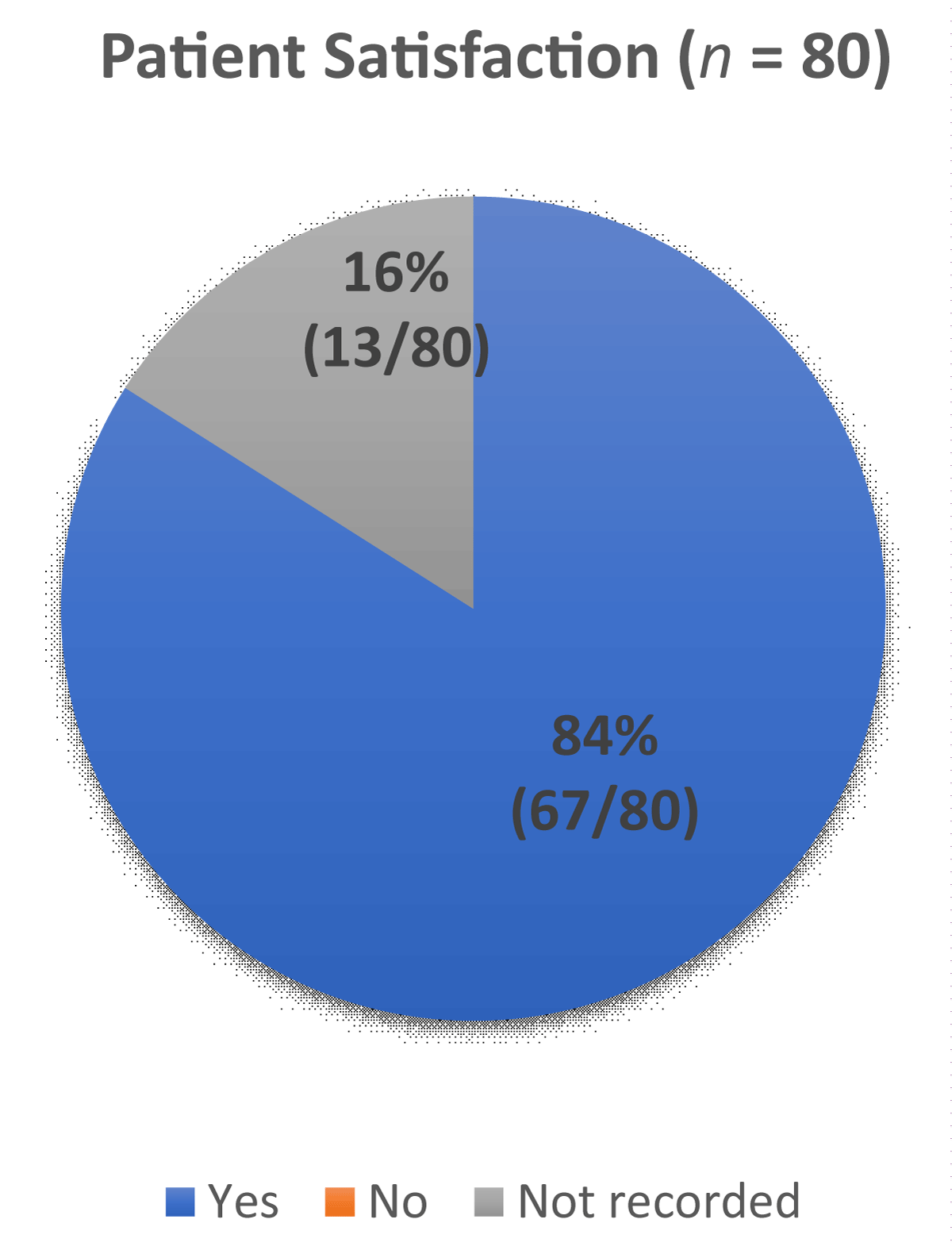
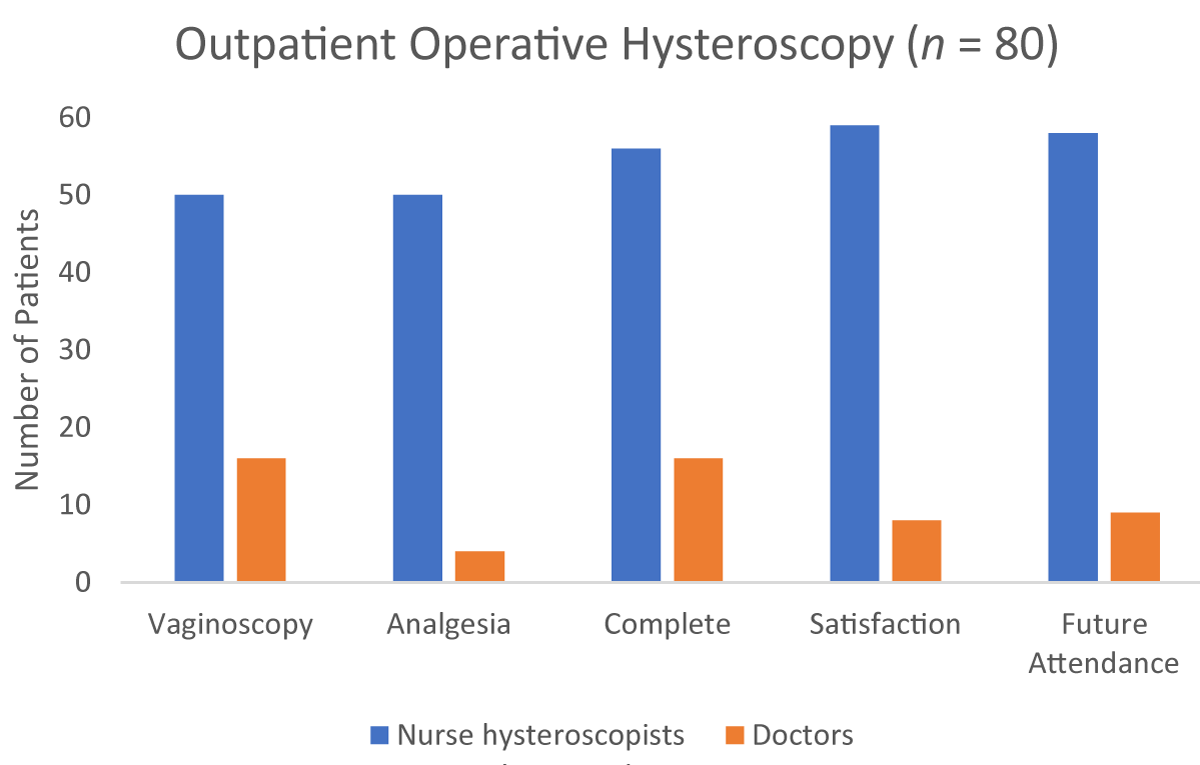
Results: In total 67/80 (84%) patients were satisfied with the service. Nurse hysteroscopists completed most procedures 59/80 (74%). Satisfaction ratings were not recorded for 13/80 (16%) consultations, completed by doctors. There was no difference in satisfaction and complication rates between doctors and nurse hysteroscopists. A total of five patients required repeat endoscopic morcellation, three completed by doctors and two completed by nurse hysteroscopists. For this group, satisfaction and complication ratings did not change.
Conclusion: High patient satisfaction and low complication rates were found. Nurse hysteroscopists performed more procedures, providing a safe and useful service. Few patients required repeat morcellation procedures.
Uterine hysteroscopy is the gold standard investigation for abnormal uterine bleeding [1]. Traditionally operative hysteroscopy, with or without anesthesia, represented the best method to visualize the uterine cavity as well as diagnose and treat uterine lesions [1]. Outpatient or ambulatory hysteroscopy represents a “one-stop-shop” policy in-cooperating hysteroscopy, endometrial biopsy, and removal of appropriate endometrial lesions [2]. Given the advances in endoscopic technology and increased clinician training, common procedures including endometrial polypectomy and small submucous leiomyoma removal can be performed in this setting [3]. Miniature hysteroscopic morcellators or Truclear devices represent one such advancement [3]. This endoscopic device mechanically removes endometrial polyps or small submucous leiomyomas [3]. Systematic reviews and meta-analysis show that morcellation of uterine polyps is associated with shorter operating time, quicker recovery and is acceptable to women [4-6].
Since 2007, outpatient hysteroscopy is available in a dedicated area in Cork University Maternity Hospital, Ireland. Services provided include uterine polypectomies, small leiomyoma removal and retrieval of intrauterine devices. Initially, this service was consultant-led. However, nurse hysteroscopists, who completed the Nurse Hysteroscopy Course, accredited by the British Society for Gynaecological Endoscopy (BSGE), have extended the capacity of this service. Irish and British Governments have developed policies to allow nurses to complete procedures traditionally performed by doctors. In Ireland, the “Policy on the Development of Graduate to Advanced Nursing and Midwifery Practice” [7] supports the training and development of advanced nurse practitioners to meet increasing healthcare demands. Several units in Ireland provide an outpatient hysteroscopy service. Most units employ nurse hysteroscopists, however, not all nurses complete operative outpatient hysteroscopy.
Several studies report patients are satisfied to attend outpatient hysteroscopy [4,5,8-13]. Only one study reported patients were satisfied with nurse hysteroscopists performing these procedures [8]. Satisfaction can be considered as an attitude, determined by numerous healthcare-related factors [14]. Patient satisfaction influences patients’ perception of quality of care and can potentially determine healthcare behaviors [14]. In our unit, women are provided with pre-procedure information leaflets and are invited to informally provide feedback after the procedure. This feedback is imperative for future audits and to identify areas for improvement to evaluate service efficiency.
This study has several aims
Examine patient acceptability and satisfaction of an outpatient operative hysteroscopy service.
Assess if patient satisfaction and complication rates were operator dependent, comparing nurse hysteroscopists with doctors.
For patients who required a repeat outpatient operative hysteroscopy, did satisfaction rating change?
In this retrospective study, we examined the charts of women who attended the service over one year from 1st of March 2020 to the 1st of March 2021. Women were included if they had either an endometrial polyp or submucosal leiomyoma requiring removal in the outpatient setting. All women had signed a consent form for the procedure.
A Truclear device was used to remove and retrieve endometrial lesions. Use of vaginoscopes, cervical dilators and pre-procedure analgesia were also recorded. Immediately after the procedure patients were asked to quantify pain on a likert scale: 0 = no pain, 1-4 mild pain, 5-7 moderate pain and 8-10 severe pain. Patients were also asked to express their satisfaction with the service and if they would attend again.
Demographic data collected included: Age, body mass index (BMI), parity, menopausal status, medications, hysteroscopic and histology findings. This data was anonymized and stored on a password encrypted computer. Data was analyzed on Microsoft Excel. The Royal College of Obstetricians and Gynaecologists (RCOG) Green-top Guideline number 59. “Best practice in outpatient hysteroscopy” [2] was used as the audit standard.
In total 80 women attended the service during the defined study period (Table 1). The mean age of this group was 53 years. Over half (n = 52/80) of women were menopausal. Women tended to be classified as obese (n = 35/80) and multiparous having had exclusive vaginal deliveries (n = 52/80). Indications for referral were mainly for post-menopausal bleeding (n = 40/80) and heavy menstrual bleeding (n = 31/80). Histology samples were largely benign (n = 73/80).
| Table 1: Baseline characteristics (n = 80). | |
| Age (years) | |
| Mean (range) | 53.3 (28-90) |
| Menopausal status | |
| Premenopausal Postmenopausal |
38 (48%) 42 (52%) |
| BMI (kg/m2) | |
| Average (range) Underweight Normal Overweight Class I obese Class II obese Class III obese Unknown |
30.2 (16.4-64.9) 3 (3.8%) 18 (22.5%) 24 (30%) 9 (11.3%) 8 (10%) 15 (18.8%) 3 (3.8%) |
| Parity | |
| Nulliparous Multiparous |
14 (18%) 66 (82%) |
| Mode of delivery (n = 66) | |
| Vaginal delivery Caesarean section Vaginal delivery & caesarean section |
52 (79%) 8 (12%) 6 (9%) |
| Indication for referral | |
| Heavy menstrual bleeding Intermenstrual bleeding Post-menopausal bleeding Incidental finding Previous partial removal of fibroid/polyp |
31 (39%) 2 (2.5%) 40 (50%) 4 (5%) 3 (3.8%) |
| Histology | |
| Benign Endometrial cancer Insufficient sample |
73 (91%) 5 (6.3%) 2 (2.5%) |
Satisfaction ratings were high: 67/80 (84%) patients were satisfied with the service and would attend the service again (Figure 1). No responses were recorded for 13/80 (16%) patients and one patient did not wish to attend the service in the future. A total of 66/80 (83%) patients had complete procedures and 9/80 (11%) hysteroscopies were abandoned (Figure 2). Reasons for abandonment were poor visualization (n = 6) and fibrous fibroids inappropriate for morcellation (n = 3).
Figure 1: Patient Satisfaction (n = 80).
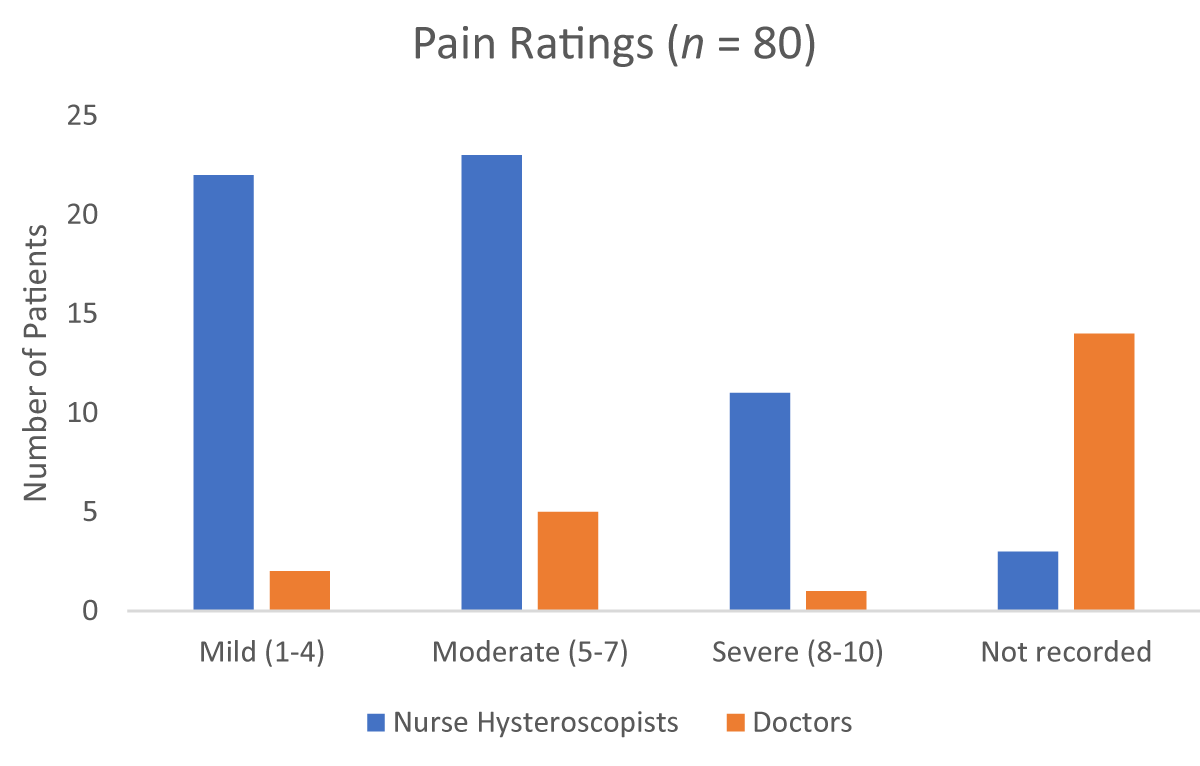
Nurse hysteroscopists completed 59/80 procedures and doctors 21/80 (Figures 2,3). For hysteroscopies completed by nurse hysteroscopists, vaginoscopy (n = 50/59) was mainly utilized. Most of these patients reported mild pain (n = 22/59), consumed pre-procedural analgesia, (n = 57/59) and were satisfied with the service (n = 59/59) and happy to attend again (n = 58/59). Complications were minimum with two patients having vasovagal responses. Doctors did not record pain levels (n = 14/21), consumption of pre-procedural analgesia (n = 10/21), satisfaction (n = 13/21) and future service attendance (n = 12/21) for most patients. Most procedures were complete (n = 14/21) with one patient having a vasovagal response.
Figure 2: Outpatient Operative Hysteroscopy (n = 80).
Figure 3: Pain Ratings (n = 80).
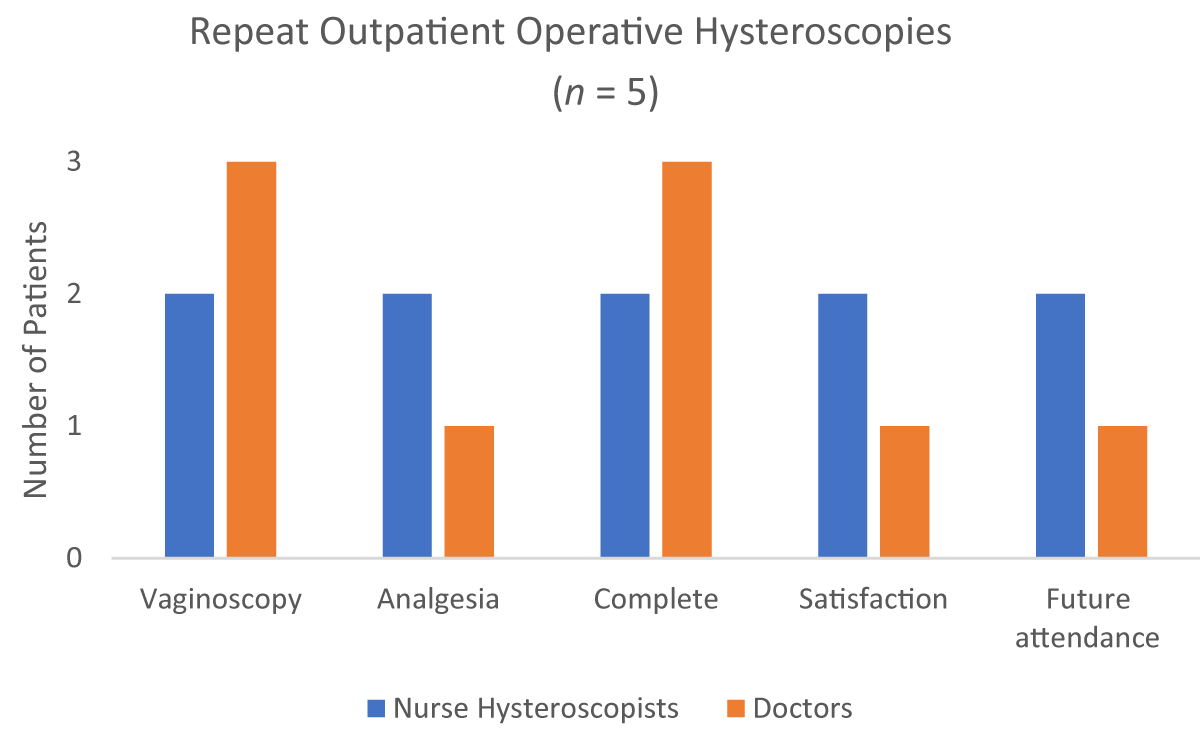
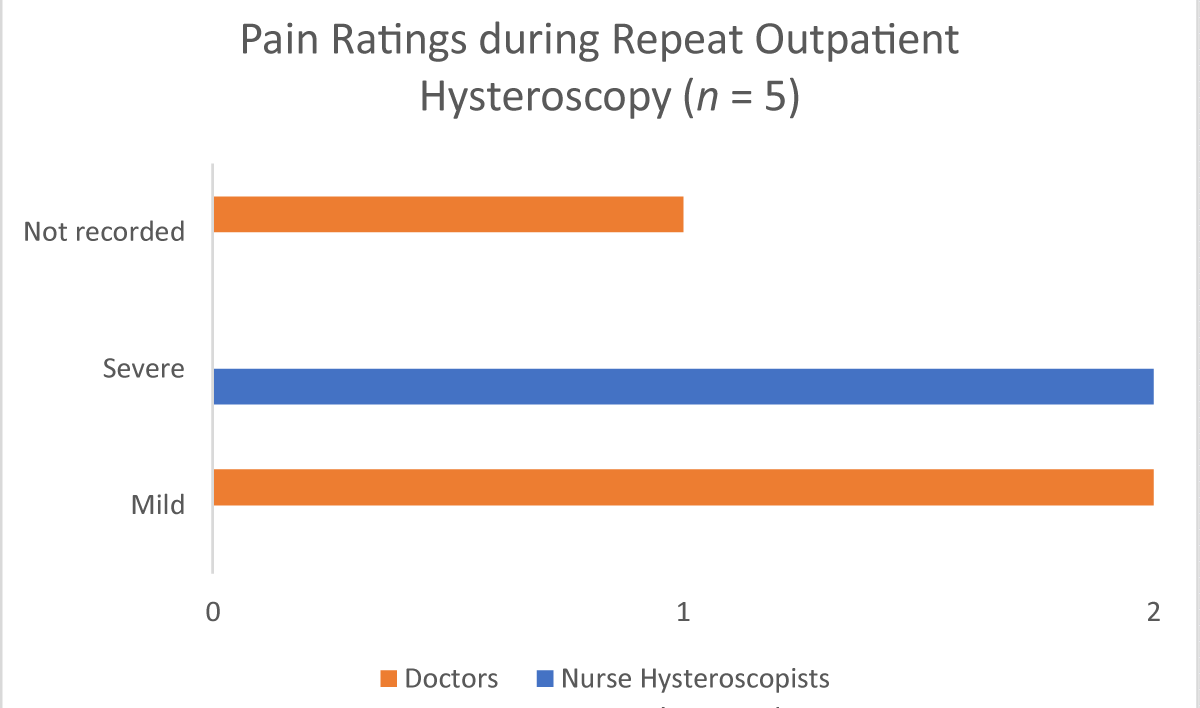
In total five patients required repeat outpatient hysteroscopies: three completed by doctors and two by nurse hysteroscopists (Figures 4,5). Morcellations were repeated to completely remove fibroids (n = 5/5). All hysteroscopies were completed via vaginoscopy and there were no complications. Satisfaction and future attendance desire did not change.
Figure 4: Repeat Outpatient Operative Hysteroscopies (n = 5).
Figure 5: Pain Ratings during Repeat Outpatient Hysteroscopy (n = 5).
This study demonstrated high patient satisfaction ratings and minimal complications. Nurse hysteroscopists provide a safe and useful service, with patients reporting 100% satisfaction ratings. Doctors frequently did not record pain, pre-procedural analgesia consumption, and satisfaction which clearly affected results. No change in satisfaction and complication rates were found in the five patients who required repeat morcellation.
Clearly outpatient hysteroscopy is a valuable resource. Post-menopausal bleeding was the most common indication for referral. These patients require prompt investigation to rule out endometrial carcinoma especially on a background of co-morbidities including elevated BMI [1,2]. Nurse hyster-oscopists completed more procedures, increasing service provision resulting in reduced waiting times. Given the increased demands on the current health system, extending scope of practice of nurse hysteroscopists is essential to ensure timely diagnosis, service efficiency and cost-effectiveness [15].
Satisfaction is multi-factorial, determined by various healthcare and non-healthcare factors [14]. In healthcare, satisfaction is defined as an evaluation of distinct healthcare dimensions [14]. Although our study found patients were satisfied with the service, provided mainly by nurse hysteroscopists, specific healthcare-related components were not assessed. Previous studies found quick recovery and convenience allowing a return to usual activities largely determined satisfaction with outpatient hysteroscopy [4,9,11-13,16]. Pre-procedural anxiety is high in most patients awaiting outpatient hysteroscopy [10,17]. However, it is unclear whether this anxiety is caused by fear of potential pathology or the procedure. To overcome this anxiety, patients reported communication and education were determinants in reducing pre-procedural anxiety, in turn decreasing dissatisfaction [11,17]. It is likely these components may have contributed to our high satisfaction result. Reassuringly, 79/80 patients – even those who required procedures – were happy to attend the service in the future.
Most patients who underwent hysteroscopies completed by nurse hysteroscopists reported mild to moderate pain. Timed consumption of pre-procedural analgesia and vaginoscopy approach were mostly compliant with RCOG guideline recommendations [2]. Although these practices may have contributed to reduced pain, previous studies found pain was not significant in determining patient satisfaction [9-11,17]. It appears the benefits of quick recovery, avoidance of general anesthesia and resumption of normal activities outweigh the disadvantage of pain or discomfort associated with outpatient hysteroscopy [9-11]. Essentially outpatient hysteroscopy and morcellation is a well-tolerated procedure, irrespective of the operator. Findings from this study, although affected by missing data from doctors, favour the role of nurse hysteroscopists performing both outpatient hysteroscopy and morcellation procedures.
To date, only one study has examined patient satisfaction with outpatient hysteroscopy performed by nurse hysteroscopists [8]. Bodle, et al. compared patient satisfaction across two separate years. Waiting time and professional skills of healthcare workers were the main determinants of patient satisfaction. Like our study, high satisfaction rates > 95% were observed in both years. This study indicates nurse hysteroscopists providing these services are skilled and safe in performing these procedures. Further studies should evaluate specific healthcare components determining patient satisfaction, comparing doctors to nurse hysterocopists.
Lastly, this study was limited by the retrospective design, small sample size and missing data. As a result of this missing data, full statistical comparison of doctors with nurse hysteroscopists was not possible, limiting study findings. However, findings from this study provide an important starting point to identify the important role of nurse hysteroscopists. Future studies should be prospective in design, including patient questionnaires in larger sample sizes to clarify specific domains determining patient satisfaction for a detailed service evaluation.
In conclusion, this study found high satisfaction and low complication rates. All patients, except one, would be happy to attend the service in the future. Nurse hysteroscopists completed more morcellation procedures. This did not affect complication or satisfaction ratings, indicating nurse hysteroscopists are safe and skilled practitioners . Few patients required repeat procedures. Although this study found 100% patient satisfaction with the service, it is unclear what specific healthcare and service-related components contributed to this finding. Future studies should aim to define these specific domains to ensure continued service efficiency.
- Cooper NA, Clark TJ. Ambulatory hysteroscopy. Obstet Gynaecol. 2013; 15: 159-166.
- Royal College of Obstetricians and Gynaecologists. Green-Top-Guidelines. Best Practice in Outpatient Hysteroscopy. Guideline No. 59. 2011.
- Ceci O, Franchini M, Cannone R, Giarrè G, Bettocchi S, et al. Office treatment of large endometrial polyps using truclear 5C: Feasibility and acceptability. J Obstet Gynaecol Res. 2019; 45: 626-633. PubMed: https://pubmed.ncbi.nlm.nih.gov/30506805/
- Downes E, Al-Azzawi F. How well do perimenopausal patients accept outpatient hysteroscopy? Visual analogue scoring of acceptability and pain in 100 women. Eur J of Obstet Gynecol Reprod Biol. 1993; 48: 37-41. PubMed: https://pubmed.ncbi.nlm.nih.gov/8449260/
- Li C, Dai Z, Gong Y, Xie B, Wang B. A systematic review and meta‐analysis of randomized controlled trials comparing hysteroscopic morcellation with resectoscopy for patients with endometrial lesions. Int J Gynecol Obstet. 2017; 136: 6-12. PubMed: https://pubmed.ncbi.nlm.nih.gov/28099700/
- Nathani F, Clark TJ. Uterine polypectomy in the management of abnormal uterine bleeding: a systematic review. J Minim Invasive Gynecol. 2006; 13: 260-268. PubMed: https://pubmed.ncbi.nlm.nih.gov/16825064/
- Department of Health. A Policy on the Development of Graduate to Advanced Nursing and Midwifery Practice. Dublin, Ireland. The Stationary Office. 2019. https://www.gov.ie/en/publication/96ce55-a-policy-on-the-development-of-graduate-to-advanced-nursing-and-midw/
- Bodle JF, Duffy SR, Binney DM. Patient satisfaction with outpatient hysteroscopy performed by nurse hysteroscopists. Int J Gynecol Obstet. 2008; 103: 116-120. PubMed: https://pubmed.ncbi.nlm.nih.gov/18760412/
- Naidu A. Factors affecting patient satisfaction and healthcare quality. Int J Health Care Qual Assur. 2009; 22: 366-381. PubMed: https://pubmed.ncbi.nlm.nih.gov/19725209/
- Gupta JK, Clark TJ, More S, Pattison H. Patient anxiety and experiences associated with an outpatient “one-stop”“see and treat” hysteroscopy clinic. Surg Endosc. 2004; 18: 1099-104. PubMed: https://pubmed.ncbi.nlm.nih.gov/15136927/
- Kremer C, Duffy S, Moroney M. Patient satisfaction with outpatient hysteroscopy versus day case hysteroscopy: randomised controlled trial. BMJ. 2000; 320: 279-282. PubMed: https://pubmed.ncbi.nlm.nih.gov/10650023/
- Roseingrave R, Lalchandani S. An Audit of Patient Satisfaction in an Outpatient Hysteroscopy Clinic Setting. Ire Med J; 114: 262.
- Boyd S, Lalchandani S. An audit on outpatient hysteroscopy–cervical dilatation, failure rates and patient satisfaction. Clin J. 2021; 4: 003-006.
- Baker R. Pragmatic model of patient satisfaction in general practice: progress towards a theory. BMJ Qual Saf. 1997; 6: 201-204. PubMed: https://pubmed.ncbi.nlm.nih.gov/10177036/
- Ludkin H, Quinn P, Jones SE, Wilkinson K. The benefits of setting up a nurse hysteroscopy service. Prof Nurse. 2003; 19: 220-222. PubMed: https://pubmed.ncbi.nlm.nih.gov/14692257/
- Morgan M, Dodds W, Wolfe C, Raju S. Women's views and experiences of outpatient hysteroscopy: Implications for a patient‐centered service. Nurs Health Sci. 2004; 6: 315-320. PubMed: https://pubmed.ncbi.nlm.nih.gov/15507052/
- Sorrentino F, Petito A, Angioni S, D’Antonio F, Severo M, et al. Impact of anxiety levels on the perception of pain in patients undergoing office hysteroscopy. Arch Gynecol Obstet. 2021; 303: 999-1007. PubMed: https://pubmed.ncbi.nlm.nih.gov/33211175/