More Information
Submitted: April 19, 2021 | Approved: April 23, 2021 | Published: April 26, 2021
How to cite this article: Sena-Martins M, Tadini V, Bolsonaro-Guilherme B, Mariani-Neto C, Pires ABN, et al. A case report of uterine inversion after home delivery. Clin J Obstet Gynecol. 2021; 4: 050-054.
DOI: 10.29328/journal.cjog.1001086
ORCiD: orcid.org/0000-0001-8762-9204
Copyright License: © 2021 Sena-Martins M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Hypovolemic shock; Uterine inversion; Hysterectomy; Huntington´s maneuver; Taxe´s Maneuver
A case report of uterine inversion after home delivery
Sena-Martins M*, Tadini V, Bolsonaro-Guilherme B, Mariani-Neto C, Pires ABN, Lucato LL, Soares AN, Xavier JC, Teixeira BACB, Faro SL and Silva TB
Hospital Leonor Mendes de Barros, São Paulo, Brazil
*Address for Correspondence: Mauricio de Sena Martins, Hospital Leonor Mendes de Barros, São Paulo, Brazil, Tel: 5511981114947; Email: [email protected]
Puerperal acute uterine inversion is a rare obstetric condition observed as a serious complication during the third stage of labor. Reported as one of the causes of postpartum haemorrhage, it commonly requires quick diagnosis and surgical treatment in order to reduce morbidity and lethality. The authors describe a case of uterine inversion with hypovolemic shock after home birth, brought to Hospital Leonor Mendes de Barros. The purpose of this article is to describe a case of acute uterine inversion and its management and a review of aetiology, predictive and risk factors, diagnosis and treatment.
A 21-year-old Brazilian woman having no prenatal care and her newborn were rushed to the emergency room of Hospital Leonor Mendes de Barros by an ambulance within an hour following a home birth. The emergency report described that the patient was found lying on the bathroom floor with her newborn in a pool of blood. The newborn, who was diagnosed with cardiorespiratory arrest, was intubated and resuscitation was immediately performed. The mother showed signs of acute anemia because of blood loss and fluids had to be infused. On arriving at the hospital the newborn was put in the Neonatology unit and preliminary examination confirmed a preterm baby, 28 weeks (Capurro score), weight = 1180 g, Apgar score = 3/4. As for the mother, she was admitted in the third stage of labor by the Obstetric team. The patient´s story was told by her sister who said that it was her third pregnancy and that she hadn´t had prenatal care. The patient had been found alone at home, in pain, and contractions had started. She had then decided to call her sister who called an ambulance. When the ambulance arrived she was found bleeding in the bathroom. The examination at first showed a pale skin, cold and clammy extremities and she was also drowsy and tachypneic. Her blood pressure was inaudible with prolonged capillary refill, respiratory rate = 20 breaths per minute, heart rate = 50 beats per minute, Glasgow coma scale = 12.
Two wide-bore cannulas were inserted and blood sent for full blood count, urea and electrolytes, clotting and crossmatch. Immediate intravenous fluid was administered as volume expansion to maintain cardicac output. She was monitored and connected to a Venturi mask (5 L/min) and blood pressure was measured = 60 × 40 mmHg, heart rate = 128 bpm and pulse oximetry = 98%.
The abdominal palpation showed moderate tenderness and the uterus wasn´t palpable above the symphysis pubis. Vulvar examination showed the fundus through the vaginal introitus with large clots of blood in the vagina. The placenta had been previously removed by the patient.
Johnson´s maneuver was performed unsuccessfully in the emergency room. The patient was immediately moved to the operating room where the maneuver was attempted a second time under general anesthesia and again without success due to a cervix ring. At this moment a surgical reduction was required and laparotomy was performed revealing a complete uterine inversion with ovaries and tubes pulled down through the inverted uterus. Huntington´s procedure was carried out successfully, but uterine atony was identified and wasn´t responsive to uterotonic drugs. Hysterectomy was then performed. The procedure required three units of packed red blood cells plus five units of fresh-frozen plasma. After that she was moved to intensive care unit. The patient remained hospitalized for six days and was then discharged.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images 1-8.
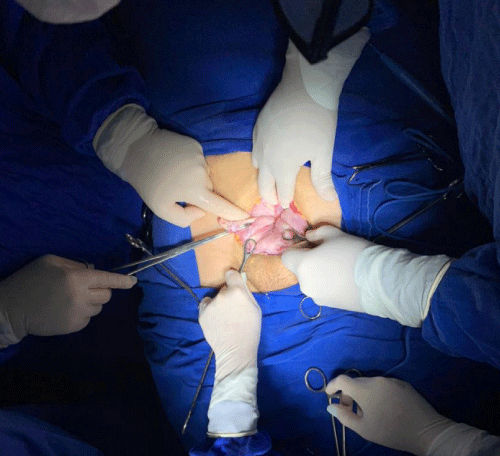
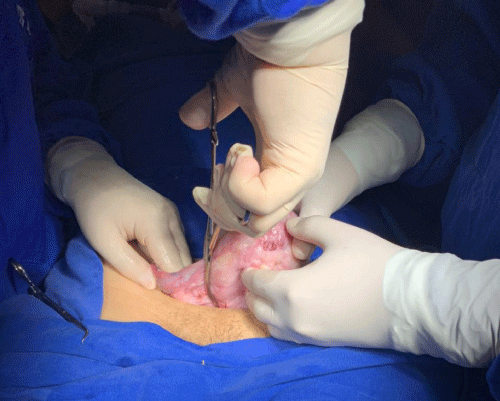
Image 1: Laparotomy aspect of Uterine inversion.
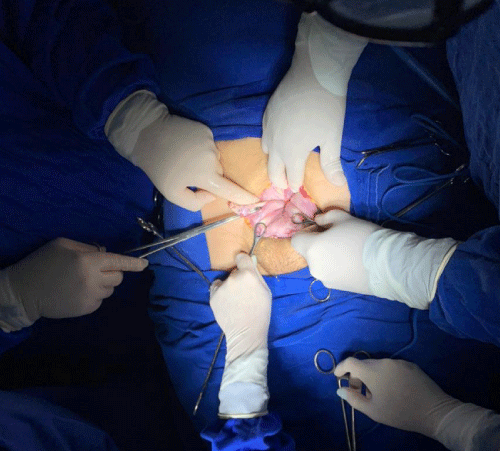
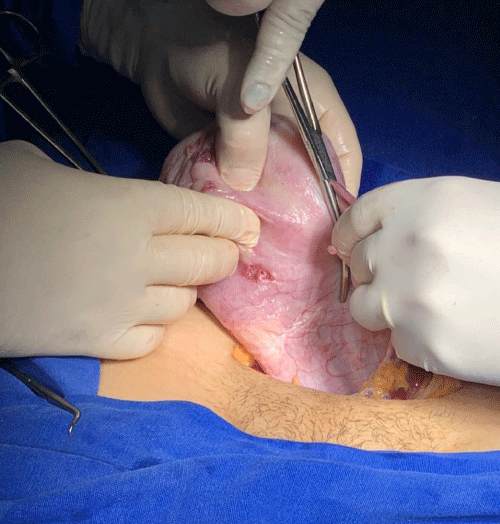
Image 2: Huntington´s procedure.
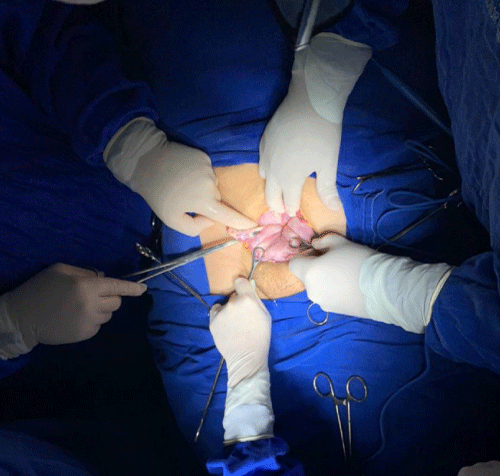
Image 3: Huntington´s procedure.
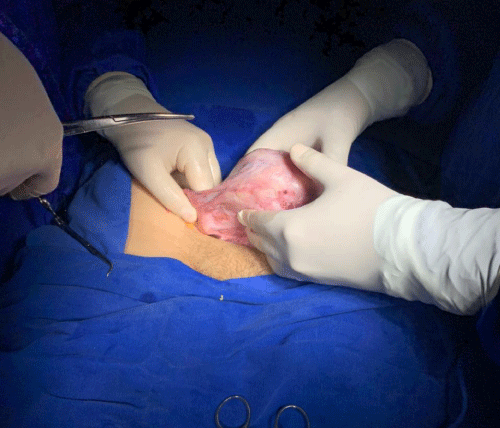
Image 4: Uterine aspect after Huntington´s procedure.
Image 5: Pale aspect of the uterus.
Image 6: Hysterectomy decision.
Image 7: Total hysterectomy.
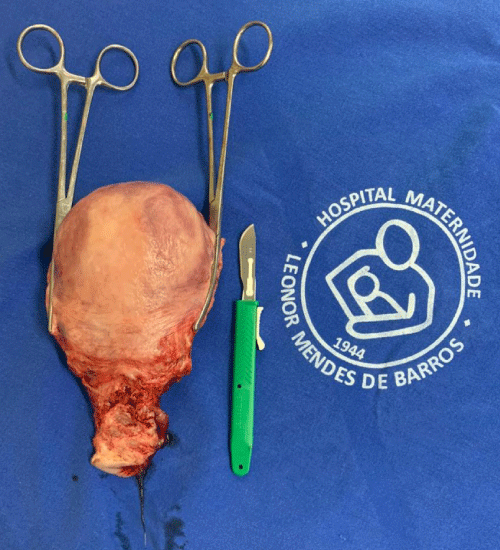
Image 8: Total hysterectomy.
Uterine inversion is a life-threatening and rare condition defined as a uterine fundus invagination through the cervix, vagina or introitus vaginal which exposes the endometrial cavity. Most cases are postpartum complications (85% to 95%) [1], but it can also occur after abortion [2]. Other than that it is rare. However, spontaneous inversion may occur frequently associated with a tumor (polyp, fibroid, sarcoma, teratoma or carcinoma) [3-5]. Mismanagement of third stage of labor may cause many cases of uterine inversion.
We present a case of acute uterine inversion after home birth at the third degree of extension. The paramedics did a good job and helped save both the mother and the newborn baby. Attempt of Johnson´s maneuver under general anesthesia was performed unsuccessfully and the general condition of the patient led to hysterectomy. We believe that this patient´s shock out of proportion to the blood loss occurred as a result of underestimated bleeding and increased vagal tone.
The reported incidence of puerperal uterine inversion ranges from 1 in 2000 to 20.000 deliveries [6-8]. In Europe it is nearly 1/100000 and 1/2000 in the USA [9]. This wide range may be related to differences in definition of inversion, postpartum assessment of the uterus, patient populations, case ascertainment and routine obstetric procedures. Brazilian data is very rare and was observed in some case reports.
The physiopathology of this condition in pregnancy may be a result of hormonal and biochemical factors which appoint ligaments laxity of the uterus and simultaneously the distension of the lower segment becoming thinner while uterine fundus become thicker because of muscle hypertrophy. Non-puerperal inversion seems to be multifactorial including intrauterine tumor rapid growth, thinning of uterine walls and distension of uterine cavity resulting in uterine cervix dilatation [5,10].
Uterine inversions are classified by the extent of inversion:
1st degree (also called incomplete) – The fundus is within the endometrial cavity 2nd degree (also called complete) – The fundus protrudes through the cervical orifice 3rd degree (also called prolapsed) – The fundus protrudes to or beyond the introitus 4th degree (also called total) – Both the uterus and vagina are inverted.
Time of occurrence (only for postpartum cases):
Acute – Within 24 hours of delivery Subacute – More than 24 hours, but less than four weeks postpartum Chronic > 1 month postpartum [6,9].
Many risk factors for uterine inversion are well consolidated, others controversial. Some authors suggest that the event occurs mainly due to poor management of the third stage of labor, especially when it comes to active (controlled) pulling of the new umbilical cord [11,12]. Others no longer point to traction as a motivator [13]. Anyway, most cases occur in low-risk patients, in other words, due to causes extrinsic to pregnancy and/or delivery [7].
The endogenous or intrinsic risk factors include excessive extension of the uterine wall due to multiple pregnancies, macrosomia and polyhydramnios, placental abnormalities such as placenta previa, accretism, placental retention and placental implantation in the uterine fundus; umbilical cord abnormalities such as multiple loops of the cord around the neck and excessively short length; congenital or acquired uterine and cervical abnormalities; tumors; connective tissue disorders (Marfan syndrome and Ehiers-Danlos syndrome); severe preeclampsia; rapid or prolonged labor; precipitated labor in the upright position; lax uterus after the second stage; marked increase in intra-abdominal pressure; prior history of inversion and controversially, nulliparity. Exogenous or extrinsic factors include manual removal of the placenta; excessive cord traction; inadequate Crede maneuver; use of uterine relaxants; prolonged use of oxytocin or magnesium sulfate [6-8,12,14-17].
The clinical diagnosis usually includes the triad: hemorrhage, shock and pelvic pain [9]. The shock itself can be motivated by bleeding or neurogenic shock or both factors. Shock intensity is not necessarily proportional to the amount of bleeding due to the neurogenic component [9], which occurs by activation of the vagal mechanism, from the stretching of ligaments [6].
The first degree or incomplete inversion exhibits a bigger diagnostic complexity [4], because the perception of fundus wall defect on the abdominal examination and the vaginal palpation may be difficult and discrete. If the uterine inversion is complete, the fundus will be palpable or will be shown through the vaginal introitus [14].
Ultrasound can be helpful in non-puerperal or non-severe acute uterine inversion and facilitate the assessment of clinically undetectable uterine inversion or in cases of unexplained postpartum hemorrhage. Sonographic findings of uterine inversion are Y-shaped uterine cavity in the longitudinal scan or a depressed longitudinal groove from the uterine fundus to the center of the inverted part and a bull´s-eye appearance of the corpus or a hyperechoic mass in the vagina with a central hypoechoic H-shaped cavity on transverse view. (CHING E HAO) (TSANG E JING) (Pauleta, Rodrigues, Melo e Graça) [3,11,18].
Imaging tests can be helpful, but delay in diagnosis and in prompt initiation of treatment may result in increase of morbidity and lethality rates, especially when shock is associated and furthermore some patients can rapidly develop disseminated intravascular coagulation [15].
Thus, all the staff (obstetrician, anesthesiologist and nurses) must work as a team [14].
The goal of the treatment is to anatomically reposition the uterus (Taxe or Johnson maneuver) as quickly as possible in order to prevent or stop the shock. The maneuver consists of mobilizing the uterine fundus with the palm of the hand and the thumb up toward the umbilical scar in the inverted area; after a successful procedure, the handle should remain in its intracavitary position until the onset of uterine contractions from the administration of uterotonics, which is performed in order to avoid reinversion and reduce volume loss. If the attempt is ineffective, drugs that relax the uterine muscle should be used in order to perform a new restitution maneuver. In case it is unsuccessful, the next step is surgery [9,13].
The arsenal of uterolytic drugs includes intravenous infusion of terbutaline, magnesium sulfate or nitroglycerin; inhaled medications such as halothane, sevoflurane and desflurane may also be used [1,14]. When a surgical approach is needed, general anesthesia with volatile anesthetics can be very useful, since the onset of action and maintenance are fast and therefore appropriate for emergency situations that require rapid uterine relaxation. Besides that, the rapid lavage makes slight contraction of the uterus possible when hypotonia is no longer essential. The inhibitory potency of sevoflurane and desflurane is comparable to that of halothane, which is a “uterorelaxant” par excellence [1,14,20].
Although the surgical stage is the last resort, there are some other non-invasive methods, with greater availability in large centers that are also effective. Among them are the Bakri Balloon and the obstetric suction cups with hydrostatic pressure.
The technique of hydrostatic pressure was described by O´Sullivan in 1945 and modified by Ogueh & Ayida in 1997. This modification introduced the suction cup and allowed the success of the method. The procedure consists of using a silastic suction cup [21] in the vagina coupled with a flow of saline solution. The accumulation of this solution generates gradual hydrostatic pressure so as to reduce the inverted uterus [22]. The size of the suction cup used can be adapted to the size of the vagina so that any leakage is effectively blocked.
The Bakri Balloon acts by hydrostatic pressure as well. It inverts the organ and keeps it normopositioned for a period that may extend up to 24 hours in order to prevent a new inversion. Success demonstrated by [6], and Majd HS [21,23].
The surgical approach can be done by laparotomy or laparoscopy. Huntington´s surgical method clamps the round ligaments below the depression, formed by the inverted uterus and tractions them until all the inversion is corrected [1,14]. Obstetric suction cups can be used in abdominal corrections instead of clamps, as shown by Antonelli, in order to be less harmful to the round ligaments during traction [24]. If it fails, the Haultain technique can be tried, which performs a longitudinal hysterotomy in the posterior portion of the median uterine wall, inferior, of 5-6 cm, reaching the inversion cervical ring, which facilitates disinvagination [1,14]. If the incision is made in the anterior wall, it is called Ocejo´s technique [1,14,25].
In order to avoid hysterectomy, some of the uterine compression sutures used in the treatment of postpartum hemorrhage serve as prophylaxis of recurrence of uterine inversion, right after the Huntington maneuver [26]. Hayman´s technique performs two or more longitudinal sutures from the anterior uterine wall to the posterior uterine wall. The entry site of the stitches should be just above the lower segment of the uterus, in its median region [27]. The Matsubara-Yano (MY) suture makes five simple loops, three longitudinal and two transverse, all anchored in a way that promotes the opposition of the uterine walls. The transverse loops are applied externally to the ends of the longitudinal loops, wrapping around them. In this way, the MY suture prevents the medial and lateral slippage that Hayman can offer for the longitudinal sutures [28].
Laparotomy has the advantage of easy conversion to hysterectomy, but it is a procedure that requires a large incision, which generates greater postoperative pain and consequently longer hospitalization [12]. Besides that, the risk of adhesions is much higher, which can complicate in subsequent pregnancies due to the increased risk of uterine rupture [25]. The laparoscopic approach requires more infrastructure, surgical experience and hemodynamic stability of the patient, but with minimal trauma, and has a more favorable postoperative with fewer complications and less pain [12]. Therefore, whenever possible, the laparoscopic approach is preferred.
Vaginal procedures include Spinelli´s and Kustner´s technique and are used mainly in non puerperal conditions [1,6,24,25].
The consensus of most authors points towards hysterectomy as the last resort because of its bleeding and infectious complications [29]. However this procedure should be rethought in critical or shock patients. Even if maternal deaths seem to be rare in well-equipped hospitals, uterine inversion is still seen especially in developing countries.
Our report describes an unassisted home birth, in which mother and newborn were primarily rescued by paramedics. Radical treatments may be reduced if the patient is rescued promptly by a qualified team of paramedics with knowledge of the third stage of labor. However the unpredictability of this condition may lead to hysterectomy.
- Neves J, Cardoso E, Araújo C, Santo S, Gonçalves P, et al. Inversão uterina. 2006; 19: 181-184.
- Mishra S. Chronic Uterine Inversion Following Mid-Trimester Abortion. Journal of Obstetrics and Gynecology of India. 2018; 68: 320–322. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6046678/
- Zohav E, Eyal Y. Anteby EY, Grin L. 2018. U‑turn of uterine arteries: a novel sign pathognomonic of uterine inversion. J Ultrasound. 2018; 23: 77–79. https://link.springer.com/article/10.1007/s40477-018-0319-0
- Bohoussou E, Dia L, Yao I, Anzoua K, Guie P, et al. Management of an Unusual Complication of Uterine Fibroids in the Gynecological Department of the University and Hospital Center of Treichville (Cote D’ivoire): About 2 Cases of Non-Puerperal Uterine Inversion. Open J Obstetr Gynecol. 2017; 7: 220-225. https://www.scirp.org/journal/paperinformation.aspx?paperid=74238
- Occhionero M, Restaino G, Ciuffreda M, Carbone A, Sallustio G, et al. Uterine inversion in association with uterine sarcoma: a case report with MRI findings and review of the literature. Gynecologic Obstetric Investigat. 2012; 73: 260-264. PubMed: https://pubmed.ncbi.nlm.nih.gov/22377482/
- Ida A, Ito K, Kubota Y, Nosaka M, Kato H, et al. Successful Reduction of Acute Puerperal Uterine Inversion with the Use of a Bakri Postpartum Balloon. Case Rep Obstetr Gynecol. 2015; 2015: 1-5. https://www.hindawi.com/journals/criog/2015/424891/
- Witteveen T, van Stralen G, Zwart J, van Roosmalen J. Puerperal uterine inversion in the Netherlands: a nationwide cohort study. Acta Obstetricia et Gynecologica Scandinavica. 2013; 92: 334–337. PubMed:https://pubmed.ncbi.nlm.nih.gov/22881867/
- Coad SL, Dahlgren LS, Hutcheon JA. Risks and consequences of puerperal uterine inversion in the United States, 2004-2013. Am J Obstetr Gynecol. 2017; 217: P377. E1-377.E6. https://www.ajog.org/article/S0002-9378(17)30627-0/abstract
- Adjoby R, Kakou C, Kouame A, Kouame N’, Abouna D, et al. Hysterectomy for Uterine Inversion: About Two Cases at University Hospital of Cocody (Abidjan—Ivory Coast). Open J Obstetr Gynecol. 2018; 8: 368-375. https://www.scirp.org/pdf/OJOG_2018041614594084.pdf
- Gonçalves ER, Bezerra LRPS, Karbage SAL, Rocha AP. Inversão uterina não puerperal em paciente jovem por mioma parido gigante: relato de caso e revisão de literatura. Revista de Medicina da UFC. 2016; 56: 58-62. http://periodicos.ufc.br/revistademedicinadaufc/article/view/19813
- Pauleta JR, Rodrigues R, Melo MA, Graça LM. Ultrasonographic diagnosis of incomplete uterine inversion. Ultrasound Obstetr Gynecol. 2010; 36: 260-261. https://obgyn.onlinelibrary.wiley.com/doi/10.1002/uog.7735
- Shepherd LJ, Shenassa H, Singh SS. Laparoscopic management of uterine inversion. J Minim Invasive Gynecol. 2010; 17: 255-257. PubMed: https://pubmed.ncbi.nlm.nih.gov/20226420/
- Tharaux CD, Sentilhes L, Maillard F, Closset E, Vardon D, et al. Effect of routine controlled cord traction as part of the active management of the third stage of labour on postpartum haemorrhage: multicentre randomised controlled trial (TRACOR). 2013; 346: f1541. PubMed: https://pubmed.ncbi.nlm.nih.gov/23538918/
- Zugaib M. Zugaib Obstetrícia. Barueri(SP). Editora Manole. 2020; 1406.
- Ihama Y, Fukasawa M, Ninomiya K, Miyazaki T. Acute puerperal uterine inversion. Foren Sci Med Pathol. 2013; 10: 272-274. PubMed:https://pubmed.ncbi.nlm.nih.gov/24356804/
- Baskett TF. Acute uterine inversion: a review of 40 cases. J Obstet Gynaecol Canada. 2020; 24: 953-956. https://www.jogc.com/article/S1701-2163(16)30594-1/abstract
- Wendel MP, Shnaekel KL, Magann EF. Uterine Inversion: A Review of a Life-Threatening Obstetrical Emergency. Obstet Gynecol Surv. 2018; 73: 411-417. PubMed: https://pubmed.ncbi.nlm.nih.gov/30062382/
- Hu CF, Lin H. Ultrasound diagnosis of complete uterine inversion in a nulliparous woman. Acta Obstetricia et Gynecologica Scadinavica. 2012; 91: 379-381. PubMed: https://pubmed.ncbi.nlm.nih.gov/22122794/
- Baggieri RAB, Vicente GS, Santos JA, Cabalero MHC, Barbosa HM, et al. Hemorragia pós-parto: prevenção e tratamento. Arquivos Médicos dos Hospitais e da Faculdade de Ciências Médicas da Santa Casa de São Paulo. 2011; 56: 96-101. http://arquivosmedicos.fcmsantacasasp.edu.br/index.php/AMSCS
- Yoo KY, Lee JC, Yoon HM, Shin MH, Kim SJ, et al. The effects of volatile anesthetics on spontaneous contractility of isolated human pregnant uterine muscle: a comparison among sevoflurane, desflurane, isoflurane, and halothane. Anesth Analge. 2006; 103: 443–447. PubMed: https://pubmed.ncbi.nlm.nih.gov/16861431/
- Majd HS, Pilsniak A, Reginald PW. Recurrent uterine inversion: a novel treatment approach using SOS Bakri balloon. BJOG. 2009; 116: 999-1001. PubMed: https://pubmed.ncbi.nlm.nih.gov/19522802/
- Tan KH, Luddin NSY. Hydrostatic reduction of acute uterine inversion. Int J Gynecol Obstet. 2005; 91: 63-64. PubMed: https://pubmed.ncbi.nlm.nih.gov/16040034/
- Thakur M, Thakur A. Stat Pearls Publishing LLC. Uterine inversion. Treasure Island (FL). 2021. PubMed: https://www.ncbi.nlm.nih.gov/books/NBK525971/
- Antonelli E, Irion O, Tolck P, Morales M. Subacute uterine inversion: description of a novel replacement technique using the obstetric ventouse. BJOG. 2006; 113: 846-847. PubMed: https://pubmed.ncbi.nlm.nih.gov/16827772/
- Sardeshpande NS, Sawant RM, Sardeshpande SN, Sabnis SD. Laparoscopic correction of chronic uterine inversion. J Minim Invasive Gynecol. 2009; 16: 646-648. https://www.sciencedirect.com/
- Alves ALL, Silva LB, Melo VH. Use of uterine compression sutures in postpartum hemorrhage. FEMINA. 2014; 42: 265-276. https://pesquisa.bvsalud.org/portal/resource/pt/lil-749147
- Mondal PC, Ghosh D, Santra D, Majhi AK, Mondal A, et al. Role of Hayman technique and its modification in recurrent puerperal uterine inversion. J Obstet Gynaecol Res. 2012; 38: 438–441. PubMed: https://pubmed.ncbi.nlm.nih.gov/22379624/
- Matsubara S, Baba Y. MY (Matsubara-Yano) uterine compression suture to prevent acute recurrence of uterine inversion. Acta Obstetricia et Gynecologica Scandinavica. 2012; 92: 734-735. PubMed: https://pubmed.ncbi.nlm.nih.gov/22881712/
- Giongo MS, Azzi T, Gios TS, Rosa TSC. Óbito pós inversão uterina: relato de caso. Arquivos Catarinenses de Medicina. 2012; 41: 79-81. http://www.acm.org.br/revista/pdf/artigos/933.pdf