Procedure
Thirteen steps for office hysteroscopy with minimal discomfort

Ricardo Bassil Lasmar1* and Bernardo Portugal Lasmar2
1Associated Gynecology Professor of Department of General Surgery and Speciality of Federal Fluminense University , UFF, Niterói, Rio de Janeiro, Brazil
2Department of Gynecology, Estacio de Sá University (UNESA),Rio de Janeiro, Brazil
*Address for Correspondence: Ricardo Bassil Lasmar, MD, PhD., Associated Gynecology Professor of Department of General Surgery and Speciality of Federal Fluminense University, UFF, Niterói, Rio de Janeiro, Brazil, Tel: +55 21 999875354; Email: [email protected]
Dates: Submitted: 18 June 2019; Approved: 26 June 2019; Published: 27 June 2019
How to cite this article: Lasmar RB, Lasmar BP. Thirteen steps for office hysteroscopy with minimal discomfort. Clin J Obstet Gynecol. 2019; 2: 034-037. DOI: 10.29328/journal.cjog.1001021
Copyright License: © 2019 Lasmar RB, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
The Office hysteroscopy (OH) is a important procedure to make diagnosis and sometimes, treatment, of intrauterine pathology, without getting the patient to Operating Room. Its advantages are very well known: less costs, fast diagnosis, see and treat and several others. It's mainly difficulty is the discomfort during the procedure. To stimule to grow the number of gynecologist to leave OR and to go to office hysteroscopy, we propose thirteen steps for office hysteroscopy with minimal discomfort.
Introduction
Office hysteroscopy (OH) is not possible for all patients and is not suitable for all hysteroscopy services. Undoubtedly, OH offers advantages over hospital diagnostic hysteroscopy (DHH), lower cost, faster result, does not remove the patient from its activities, a short exam time of 2 to 5 minutes and, in cases of synechia, reduces the risk of false pertuit and perforation, because there is pain referred by the patient when it leaves the surgical plane of the fibrosis. In addition, most diagnostic hysteroscopies are normal, that is, they do not find pathologies. However, the pain and discomfort factor are important issues, which lead the patient to decide on procedure under anesthesia. As for the gynecologist, the training factor, calm and sometimes the financial, lead to the decision of the patient’s hospitalization [1,2].
For those who are interested in office hysteroscopy, it is known that the limit of acceptable discomfort is individual, each patient has his, and this should always be respected by the examiner. The use of scopolamine butylbromide 30 minutes before the procedure decreases pain and the consequences of the vagal effect, and more potent anti-inflammatories and analgesics such as Ketorolac Trometamol may also be used. Some care should be taken to make office hysteroscopy with minimal discomfort:
1- Talk to the patient before the examination knowing the complaints, the reason for the examination, explaining in detail how the procedure will be, at which points she may feel discomfort, that she will see the inside of her uterus as well, and will understand better what is happening. Reinforce that the procedure will be immediately interrupted at the request. Warn that might have bleeding for four to seven days after the procedure. If possible show with models how the hysteroscope will progress and where it will feel discomfort. When the gynecologist demonstrates knowledge about the procedure, detailing the steps, ensuring that the discomfort will be bearable and ensuring that she will stop the procedure when she asks, the patient becomes calmer and confident. Sometimes the patient goes to the examination table with the proposal of just trying to do it and, confident, ends up managing to perform it without problem.
2- Smaller instruments. The discomfort is directly related to the diameter of the hysteroscope, being more indicated those of 6 mm or smaller. Especially in patients who did not have vaginal deliveries, postmenopausal and/ or in the elderly [3,4].
3- Hysteroscopic shirt with operative channel. The presence of an operative canal allows the biopsy of the endometrium, identified lesions or the hysteroscopic office surgery at the same moment of the investigation and without the need for an instrument change, namely, to exit and place other instruments through the transcervical route. The operative channel allows the biopsy or surgery with tweezers, scissors or devices of 5 to 7 FR, being biopsy with forceps more precise and much less uncomfortable than the one with Novak or curette that, sometimes, need speculum placement [5,6].
4- Vaginal touch facilitates the identification of the position of the cervix and the uterine body, especially in the cases of a very anterior or posterior cervices, as well as in pronounced anteversoflections or uterine retroversions. This reduces the movement of the hysteroscope in the vagina at the beginning of the procedure.
5- Patient is in gynecological position with the buttocks slightly off the gynecological table and the lower limbs well away. This position will facilitate, when necessary, the broad external movement for the minimum and smooth internal movement, with this less discomfort. In the lateralized uterus, the lower limb should be moved away from the uterine lateralisation so that there is no blockage in the movement of the hysteroscope. In pronounced anteversion, the hand will be positioned posteriorly, while in the retroversion, it will be very anterior, sometimes requiring the gynecologist to stand.
6- Hold the microcamera with the right hand (in the right-handed gynecologists, the opposite in the sinister), with support between the thumb and forefinger, with the left hand holding the light source cable, allows all movements to optimize the 30 degree optics . The change in the axis is performed with the north-south, east-west movement of the right hand and the laterality with the rotation of the light source cable, with the left hand, when positioned to the left of the examiner, one observes the left side of the uterine cavity, when positioned down the anterior wall of the uterus is evaluated. In this way, with light movements it is possible to investigate the entire uterine cavity.
7- Liquid distension media should be used as it allows the examination to be performed even when the patient has some bleeding, since abnormal uterine bleeding is the major indication of hysteroscopy. The saline distention allow the examination to be performed without placement of the vaginal speculum and clamping of the cervix with Pozzi tweezers, doing the vaginoscopy. But to minimize discomfort, you must use the lowest possible pressure that can distend the cavity in the shortest time possible for the inside of the uterus to be evaluated. The high pressure and the prolonged time of the examination will lead to greater discomfort. The gas distension medium may lead to post hysteroscopy pain because of the passage of CO2 through the tubes [7].
8- Put a monitor for the patient to follow the examination. This makes her entertained with the beauty of the image, understands the exam and participates with the gynecologist for its accomplishment. The advantage of hysteroscopy over other imaging tests is that it is possible for the patient to see, understand and participate actively, so this should be used as a facilitator of the procedure.
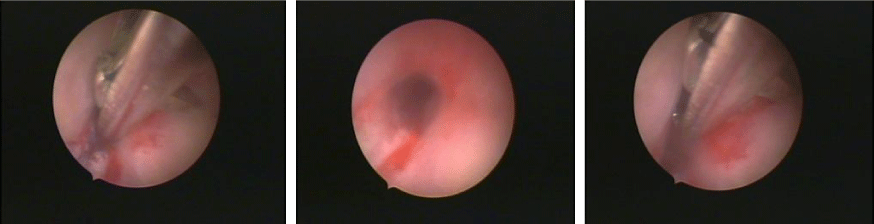
9- Section the stenoses and synechiae and do not stretch them or try to break with the force. The section of fibrotic tissue does not cause pain to the patient, while trying to overcome it with force causes great discomfort and pain, so use hysteroscopic scissors, 5 or 7 fr, to section the external and internal orifice stenosis and the fibrous intrauterine synechiae. In synechiolysis the pain reference is a probable sign of a myometrial section, that is, false pertuite, so whenever possible we try to lysis the intrauterine synechiae in outpatient hysteroscopy, without anesthesia figure 1 [8,9].
10- Pressing the pelvis reduces the discomfort of hysteroscopy. In hysteroscopy, the passage through the internal orifice represents the moment of greatest discomfort to the patient, with risk of vagal reaction. To minimize this discomfort, the coincident hysteroscope axes must be offered with those of the internal orifice. For this purpose, the hysteroscope should be placed laterally in the oval orifices, or it should be inserted with the tip of the anterior-oriented hysteroscope bevel in the pronounced anteversoflexions or posterior, in the accentuated retroversoflexions. All such rotational movement (fiber optic cable) and axis (north-south, east-west movement of the microcamera) must be performed smoothly, to be bearable. Placement of the patient’s hand in the pelvis greatly reduced the discomfort from this moment and should be maintained until the end of the procedure. This pressure in the pelvis also leads to rectification of the uterus in the anteversoflexions [9].
11- Varying intrauterine pressure, using low pressures, or emptying and replacing the fluid in the uterine cavity, allows the visualization of small lesions adhered to the wall, as well as subendometrial changes such as adenomyosis or small submucous fibroids. This dynamics allows us to perceive extrinsic compression in the uterine cavity, caused by large intramural fibroids.
12- Directed biopsy of the most representative area of the lesion allows greater diagnostic precision in the anatomopathological study and causes much less patient discomfort than conventional biopsies, curettes and Novak instruments. Aspiration cannulae would also lead to less discomfort, but for its introduction it is necessary the placement of speculum and sometimes pinching of the cervix with Pozzi, causing more discomfort and pain. Another advantage is the possibility of performing complete exeresis of the lesion when the tweezers or scissors is directed to the base of the lesion. With directed biopsy or in outpatient surgery, the removal of the material should occur with the closure of the entrance tap of the distension medium and approach of the material to the optics, with withdrawal of the entire hysteroscope together. It is important to emphasize that the material should be placed in a container with formalin by the examiner [10,11].
13 - Discharge of the distention medium at the end of the procedure - Remaining of the distention liquid medium may cause cramps to the patient, therefore, the need for complete emptying of the uterine cavity. This should be done mainly in patients with uterus with large angulations and or with very narrow paths.
Conclusion
Applying these thirteen steps, the patient will feel less pain, less discomfort and will get more safety at the hysteroscopy procedure.
References
- Cicinelli E, Parisi C, Galantino P. Reliability, feasibility, and safety of minihysteroscopy with a vaginoscopic approach: experience with 6,000 cases. Fertil Steril. 2003; 80: 199-202. Ref.: https://bit.ly/2X2Nh17
- De Angelis C, Santoro G, Re ME, Nofroni I. Office hysteroscopy and compliance: mini-hysteroscopy versus traditional hysteroscopy in a randomized trial. Hum Reprod. 2003; 18: 2441-2445. Ref.: https://bit.ly/2Fy1xsI
- Bettocchi S, Nappi L, Ceci O, Selvaggi L. What does "diagnostic hysteroscopy' mean today? The role of the new techniques.. Curr Opin Obstet Gynecol. 2003; 15: 303-308. Ref.: https://bit.ly/2YpBdZ2
- Di Spiezio Sardo A, Zizolfi B, Lodhi W, Bifulco G, Fernandez L, et al. See and treat' outpatient hysteroscopy with novel fibreoptic 'Alphascope'. J ObstetGynaecol. 2012; 32: 298-300.
- Guida M, Di Spiezio Sardo A, Acunzo G, Sparice S, Bramante S, et al. Vaginoscopic versus traditional office hysteroscopy: a randomized controlled study. Hum Reprod. 2006; 21: 3253–3257. Ref.: https://bit.ly/2XDGIpW
- Paulo AA, Solheiro MH, Paulo CO. Is pain better tolerated with minihysteroscopy than with conventional device? A systematic review and meta-analysis: hysteroscopy scope size and pain. Arch Gynecol Obstet. 2015; 292: 987-994. Ref.: https://bit.ly/2KFz5t3
- Craciunas L, Sajid MS, Howell R. Carbon dioxide versus normal saline as distension medium for diagnostic hysteroscopy: a systematic review and meta-analysis of randomized controlled trials. Fertil Steril. 2013; 100: 1709-14.e1-4. Ref.: https://bit.ly/2KGkvSi
- Mazzon I, Favilli A, Horvath S, Grasso M, Di Renzo GC, et al. Pain during diagnostic hysteroscopy: what is the role of the cervical canal? A pilot study. Eur J Obstet Gynecol Reprod Biol. 2014; 183: 169-173. Ref.: https://bit.ly/2LnZZoX
- Lasmar RB, Bruno RV, Santos RLC, Lasmar BP. Histeroscopia do Lasmar Tratado de Ginecologia. 553-564, Guanabara Koogan. 2017.
- Centini G, Troia L, Lazzeri L, Petraglia F, Luisi S. Modern operative hysteroscopy. Minerva Ginecol. 2016; 68: 126-132.
- Lasmar RB, Barrozo PRM, Oliveira MAP, Coutinho ESF. Validation of hysteroscopic view in cases of endometrial hyperplasia and cancer in patients with abnormal uterine bleeding. Journal of Minimally Invasive Gynecology. 2006; 13: 409-412. Ref.: https://bit.ly/2Ner5Bq